Cellular breakdown in the lungs claims a bigger number of lives every year than some other kind of disease around the world. As per the World Wellbeing Association, an expected 1.8 million individuals will have passed on from cellular breakdown in the lungs in 2020. Flow therapies take one of two paths: combined chemotherapy, which has harsh side effects for cancer patients, or focusing on cancers with unmistakable changes, which may not matter to many patients—both of which make fighting the illness difficult.
Scientists at SRI Global have planned and enhanced another peptide—a particle that contains at least two amino acids—to go about as a conveyance vehicle for medications to treat non-little cell cellular breakdown in the lungs, which represents most of these cases. This peptide, featured in a new report distributed in Nature Communications Science, can convey huge quantities of disease drugs and effectively target harmful cells, restricting them and setting off a cycle to draw the peptide and its freight inside.
“With our peptides, we can begin to convey huge freights within a cell that couldn’t in any case go through the cell film,” said Kathlynn Brown, SRI’s Bioscience division’s VP of medication conveyance frameworks and the paper’s lead author.”It essentially allows therapeutics to be hauled into the inward functions of cancer cells while staying away from solid cells, limiting the likely aftereffects.”
“To begin with, we do not attempt to target a specific cell surface marker. We use what’s known as unbiased selection, which basically means that we’ll let the cells tell us which answer is better. We’re not going to try to outwit nature.”
Kathlynn Brown, vice president of drug delivery systems at SRI’s Bioscience division.
As of now, most similarly designated disease drugs are conveyed by antibodies, which bind to explicit receptors on the outer layer of a malignant growth cell. Yet, there are a few benefits to utilizing peptides rather than antibodies. To start with, peptides are essentially smaller particles, and that implies that they can enter further into a growth. Second, peptides can be assembled artificially, while antibodies should be created naturally in cells. The compounding cycle is quicker, more affordable, and gives analysts more exact control over the end product.
“Since we make them synthetically, we have a ton of adaptability in the way we integrate the medication,” Brown said. “We can put on anything—medication or freight—we need; we will know precisely where it is, and we can alter that with devices we have in the lab.”
To find a peptide with the right arrangement of qualities, Brown and her partners utilize an exclusive choice cycle to filter through a library of billions of likely choices. For this situation, they required a peptide that could effectively search out and bind to disease cells while letting solid cells be; could set off organic cycles to quickly bring the peptide and its freight into the cell; and wouldn’t degrade while flowing through the body.
“We don’t attempt to focus on a specific cell surface marker regardless,” Brown said. “We do what’s alluded to as a fair choice, which essentially implies that we will let the cells let us know the most fitting response.” “We won’t attempt to outfox nature.”
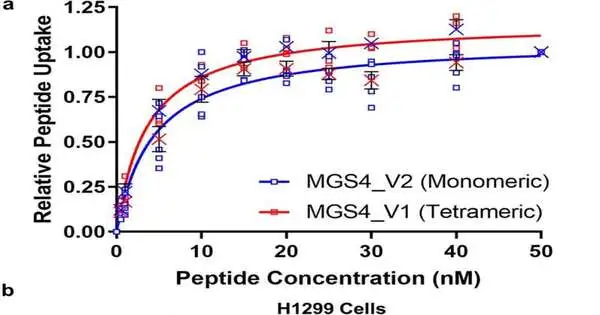
When Brown and her group recognized a peptide with the right qualities, known as MGS4, they changed it to be basically as viable as could be expected and tried it with a harmful protein called saporin, which can’t really get into cells all by itself. They discovered that MGS4 effectively conveyed saporin to cellular breakdown in mouse lungs cancers, and that after 18 days of therapy, growths in mice given saporin combined with MGS4 were a fraction of the size of growths in untreated mice or mice given saporin alone.
Their work shows the way that MGS4 could be an important device in creating designated therapeutics for cellular breakdown in the lungs. Furthermore, on the grounds that it can convey various medications, the analysts are simply starting to investigate its therapeutic potential.
“This protein poison is our most memorable helpful idea, yet what’s truly significant is that this peptide can convey huge, harmful biologic treatments within a growth cell,” Brown said. “We’re truly trusting that we can take this peptide and use it in various applications with numerous different therapeutics.”
More information: Curtis A. Allred et al, Tumor-specific intracellular delivery: peptide-guided transport of a catalytic toxin, Communications Biology (2023). DOI: 10.1038/s42003-022-04385-7
Journal information: Communications Biology