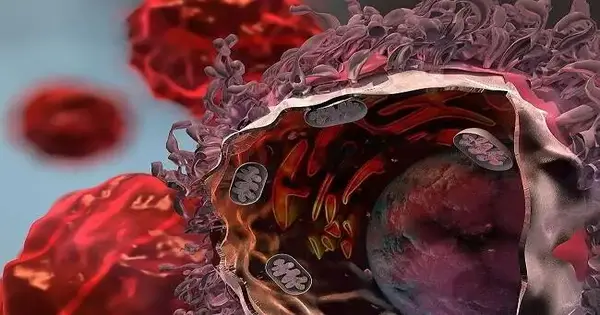
A protein usually found at undeniable levels in cellular breakdown in the lungs’ cells controls a significant immunosuppressive pathway that permits lung cancers to dodge safe assault, as per a review conducted by scientists at Weill Cornell Medicine. The disclosure could hasten the advancement of therapies that beat this growth guard system and further develop results for cellular breakdown in the lungs.
In the review, which appeared Jan. 9 in Nature Correspondences, the analysts examined human cellular breakdown in the lungs datasets and performed tests in preclinical models of cellular breakdown in the lungs to show that the transcription factor XBP1s improves growth endurance by stifling the counter-disease action of adjoining safe cells. They found that XBP1s applied this impact by driving the creation of a strong immunosuppressive particle, prostaglandin E2.
“We discovered that XBP1s are required for a critical pathway in disease cells that directs the nearby safe environment in lung growths and can be disrupted to increase anticancer resistance,” said study co-author Dr. Vivek Mittal, the Gerald J. Portage Wayne Isom Professor of Cardiothoracic Medical Procedure and head of the Neuberger Berman Cellular Breakdown in the Lungs Lab at Weill Cornell Medication.
We discovered that XBP1s can be inhibited to boost anticancer immunity since it is a component of a crucial pathway in cancer cells that controls the local immunological environment in lung tumors.
Co-senior author Dr. Vivek Mittal
The other co-senior creator of the review is Dr. Juan Cubillos-Ruiz, William J. Record, M.D., recognized academic partner for disease and immunology in obstetrics and gynecology, and co-head of the malignant growth science program at the Meyer Disease Center at Weill Cornell Medicine. The main creator is Dr. Michael Crowley, who finished his doctorate in Dr. Mittal’s lab in 2021.
There are almost 250,000 new instances of cellular breakdown in the lungs consistently in the US, and in excess of 130,000 cellular breakdown deaths, as per the American Disease Society, making this type of malignant growth the main source of disease mortality in the country. The vast majority of cases are of a type known as non-small cell cellular breakdown in the lungs (NSCLC), which is frequently studied at the cutting edge of movement.
Newer therapies that aim to destroy diseases’ safe stifling guards or attack tumors with engineered resistant cells have shown promise against other disease types, but have had extremely limited success against NSCLC.Disease analysts accept that this is because of NSCLC’s extra, unseen stifling systems. Much exploration is presently directed toward revealing and tracking down ways of destroying these extra administrative pathways.
In the review, the scientists zeroed in on the IRE1-XBP1 arm of the unfurled protein reaction, a pathway that is constantly upregulated in numerous tumors. Earlier investigations of other cancer types have found proof that this pathway not only straightforwardly advances the endurance and movement of growths, but in addition assists with stifling the antitumor action of adjacent safe cells. However, the role of the pathway in NSCLC has largely gone unnoticed.
When IRE1 is activated in cells under stress, it starts producing XBP1s, a performing various tasks record factor that controls the outflow of various quality projects in a setting explicit way.The scientists examined the articulation levels of the quality encoding XBP1s from a huge arrangement of human NSCLC tests listed in a public data set and found proof that patients whose cancers had higher XBP1s levels had more terrible possibilities of endurance. Stable with that finding, they showed that taking out IRE1 or XBP1s from NSCLC-like cancers in mice prompted growth relapse and notably further developed endurance.
Further examination uncovered that the erasure of XBP1s in NSCLC cells hinders cancer development mostly by permitting the safe framework to really go after the growth considerably more. The researchers tracked down that XBP1s, when created inside growth cells, build a firmly immunosuppressive particle called prostaglandin E2, which is emitted into the cancer microenvironment where it really stifles the anticancer action of safe cells.
The discoveries propose that crippling IRE1-XBP1s may be a decent treatment system for NSCLC and could function admirably in combination with other immunotherapy approaches.
“Focusing on IRE1-XBP1 could address a helpful, two-dimensional remedial methodology that controls cellular breakdown in the lungs’ movement while prompting the defensive enemy of cancer resistance,” said Dr. Cubillos-Ruiz.
“We are currently extremely keen on tracking down ways of focusing on an IRE1-impeding medication specifically for growth cells,” said Dr. Mittal, who is likewise an individual from the Meyer Disease Center.
As a feature of the review, the scientists likewise planned the quality action “signature” brought about by taking out IRE1 in mouse NSCLC cancers. They found that the presence of this equivalent quality mark in human NSCLC growths predicted better quiet endurance. A clinical test in view of this mark could be helpful later on for foreseeing results and choosing ideal medicines, they said.
More information: Michael J. P. Crowley et al, Tumor-intrinsic IRE1α signaling controls protective immunity in lung cancer, Nature Communications (2023). DOI: 10.1038/s41467-022-35584-9
Journal information: Nature Communications