UCLA researchers have fostered another technique to design all the more impressive invulnerable cells that might possibly be utilized for “off-the-rack” cell treatment to treat malignant growths.
“Off-the-rack” cell treatment, otherwise called allogenic treatment, utilizes resistant cells obtained from sound contributors rather than patients. The methodology can bring cell treatments, such as illusory antigen receptor (vehicle) lymphocyte treatment, to additional patients in a more ideal way, which is one of the significant hindrances in seeking these life-saving medicines from patients.
“Time is frequently of the substance with regards to treating individuals with cutting-edge malignant growths,” said Lili Yang, academic partner of microbial science, immunology, and atomic hereditary qualities and individual from the UCLA Wellbeing Jonsson Complete Disease Community. “At present, these sorts of treatments should be custom-fitted to the singular patient. We need to separate white platelets from a patient, hereditarily engineer the cells, and then re-mix them back into the patient. This cycle can take a long time to months and can cost countless dollars to treat every patient.”
“They exhibit elevated effector molecule levels and possess the capacity to carry out cellular cytotoxicity against cancer cells in an antibody-dependent manner. We discovered that we may enhance their anti-cancer qualities by employing CD16 as a biomarker for donor selection.”
Yang, who is also a member of the Eli and Edythe Broad Center of Regenerative Medicine and Stem Cell Research at UCLA
This new methodology, depicted in Nature Correspondences, is a vital step toward growing more compelling cell treatments that have a lower cost and standby that can be efficiently manufactured and delivered to medical clinics all over the planet, making vehicle lymphocyte treatment more reasonable and open to a more extensive scope of patients.
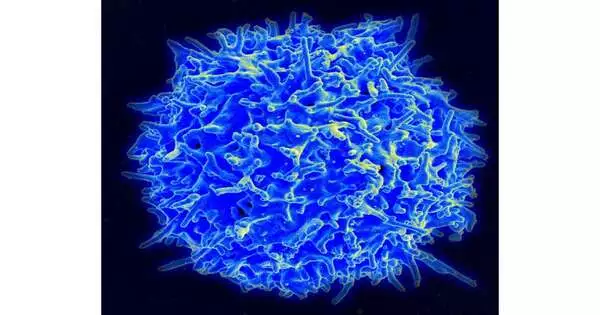
For the review, Yang and her group zeroed in on gamma delta lymphocytes, a resistant cell known for its capacity to focus on a wide exhibit of malignant growths—including strong cancers—without causing join-versus-have illness, a typical complexity in allogeneic cell treatments.
While gamma delta lymphocyte-based therapies have been concentrated previously, they have had restricted clinical accomplishment because of contributor fluctuation, brief ingenuity, and disease cells’ capacity to get away from or keep away from the body’s invulnerable reaction.
In any case, Yang and her group found that contributor gamma delta lymphocytes with high articulations of a CD16 surface marker had a more noteworthy capacity to kill malignant growth cells.
“These CD16-high gamma delta lymphocytes show exceptional qualities that build their capacity to perceive growth,” said Yang, who is likewise an individual from the Eli and Edythe Wide Focus of Regenerative Medication and Immature Microorganism Exploration at UCLA and the review’s senior creator. “They show uplifted degrees of effector atoms and are furnished with the capacity to participate in neutralizer subordinate cell cytotoxicity against malignant growth cells. We found that by involving CD16 as a biomarker for giver determination, we can further develop their enemy of malignant growth properties.”
Yang and her group likewise defeated a portion of the issues seen in past examinations with gamma delta lymphocyte therapies by designing the cells so they were outfitted with vehicle and IL-15, two fundamental parts that assist with improving gamma delta immune system microorganisms’ disease-battling capacities.
The group of researchers was then ready to productively create the more strongly designed cells in enormous amounts, which they tried on two different preclinical ovarian disease models. They found the cells were equipped for going after cancers and stayed in the models for an extensive stretch of time, empowering them to proceed with their enemy of growth impacts. Moreover, there were no indications of difficulties, for example, unite versus have illness.
“The consequences of this examination shed light on the promising plausibility, restorative potential, and striking wellbeing profile of these designed CD16-high gamma delta white blood cells,” Yang said. “We trust this can be a suitable restorative choice for malignant growth treatment later on.”
The concentrate’s most memorable creators are Derek Lee and Wenbin Guo from UCLA and Zachary Dunn from USC. Different creators incorporate Carl Rosenthal, Natalie Penn, Yanqi Yu, Kuangyi Zhou, Feiyang Mama, Miao Li, Tsuan-Ching Melody, Xinjian Cen, Yan-Ruide Li, Jin Zhou, and Matteo Pellegrini, all from UCLA, and Pin Wang from USC.
More information: Derek Lee et al, Nature Communications (2023). DOI: 10.1038/s41467-023-42619-2