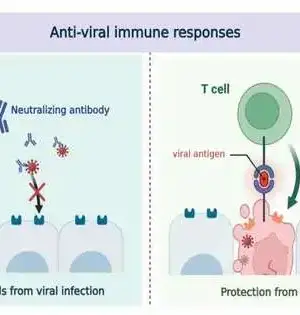
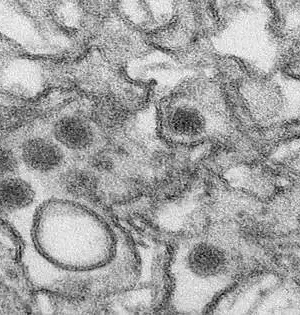
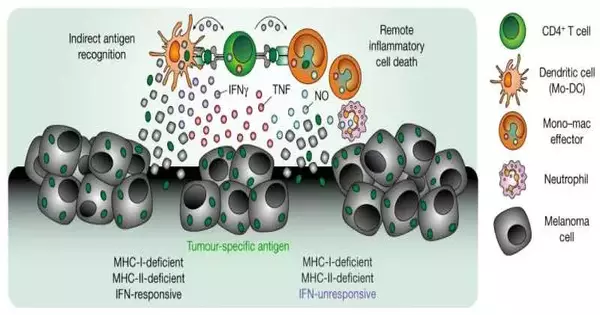
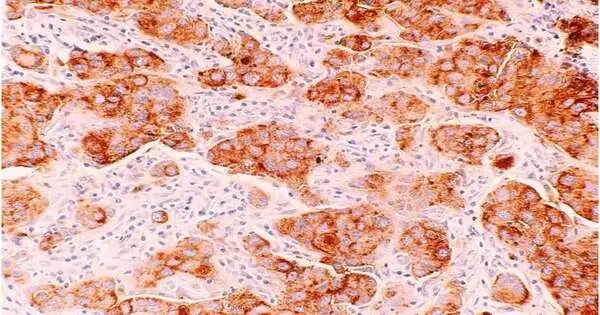
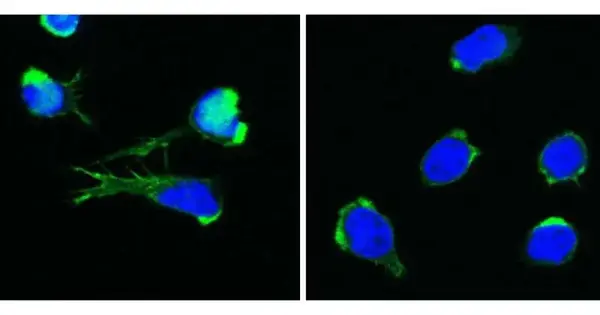
A multidisciplinary group of researchers at Magdeburg's Otto-von-Guericke University has discovered a new method by which inflammatory mediators of pathogen defense can remotely kill cancer cells, making a significant contribution to the development of better cancer immunotherapies. Immunotherapies today strengthen the body's own cancer defenses. They activate the immune system's killer T cells, which are capable of specifically recognizing and eliminating cancer cells. However, in many patients, cancer cells change and become inaccessible to killer T cells, rendering the treatment ineffective. A new mechanism that enables the immune system to also eliminate such invisible cancer cells has been discovered by
Immunology
Patients' varying responses to treatment are one of the main reasons cancer is difficult to treat. These variations are rarely anticipated. The majority of the time, administering a therapy to a patient and then waiting and watching is required to determine whether or not the patient will respond to it. That puts a lot of pressure on doctors and researchers, poses a lot of danger to cancer patients, and costs more. The most effective treatments and regimens could be tailored to each individual patient, thereby increasing the likelihood of success. Because of this, researchers have been concentrating on finding useful
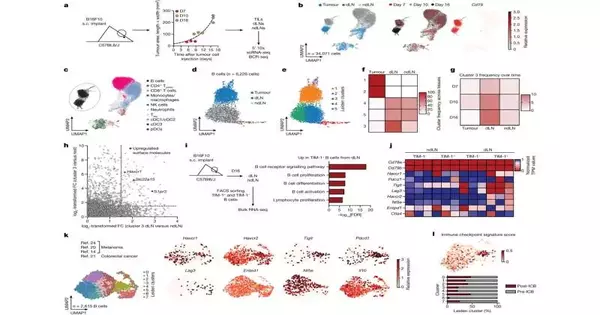
The function that B cells play in the fight against cancer has been the subject of more in-depth immunology research carried out under the direction of Harvard Medical School. The team identifies a crucial checkpoint of B-cell activation and how bypassing the checkpoint could unlock T-cell potential in a paper that was published in Nature and is titled "B-cell-specific checkpoint molecules that regulate anti-tumor immunity." Various B-cell types were studied during melanoma growth, and gene expression levels were tracked with high-throughput flow cytometry, bulk, and single-cell RNA sequencing. They discovered that melanoma tumor growth was significantly accelerated worldwide when B-cells
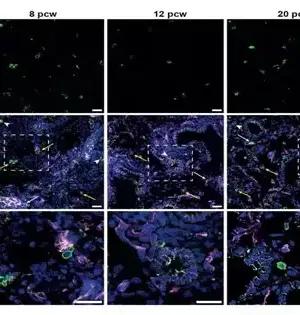
Nearby lymph nodes, which are part of the immune system, are typically the first place where cancer spreads in breast cancer. From here, cancer cells can travel to the brain, lung, liver, and bones. Cancer cells suppress anti-cancer immune responses in the lymph nodes to survive and spread, or metastasize, according to new research led by researchers at Massachusetts General Hospital (MGH). New approaches to preventing this suppression and unleashing the immune system to fight cancer may emerge from the findings, which were recently published in the Journal of Experimental Medicine. The researchers looked at and compared the gene expression
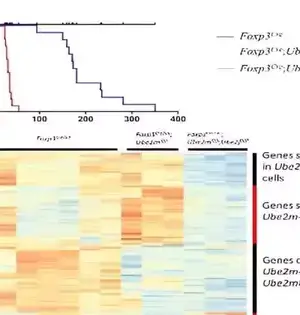
Researchers from the St. Anna Children's Cancer Research Institute, the CeMM Research Center for Molecular Medicine of the Austrian Academy of Sciences (AW), and the Medical University of Vienna have discovered a brand-new disease that links inflammation, immune system disruptions, and blood formation disruptions in their search for the cause of four children's baffling symptoms. This discovery provides the foundation for a deeper comprehension of related diseases. The researchers' recent publication in the New England Journal of Medicine marks a significant milestone. A defect in the DOCK11 gene has been found to cause both white and red blood cell abnormalities.
There is increasing evidence that astronauts are more likely to contract infections while in space. In addition to respiratory and non-respiratory illnesses, astronauts on the International Space Station (ISS) frequently suffer from skin rashes. It is also known that astronauts shed more live virus particles, for instance, the Epstein-Barr virus, varicella zoster, herpes simplex, and cytomegalovirus, which cause shingles. Space travel may weaken our immune system, according to these observations. However, what could cause such a weak immune system? Dr. Odette Laneuville, an associate professor at the Department of Biology at the University of Ottawa and the lead author of
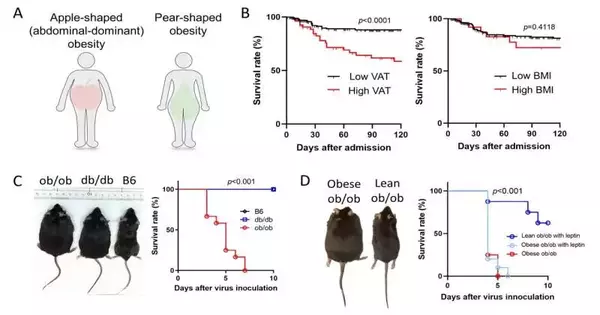
In COVID-19 patients, apple-shaped obesity is linked to cytokine storm and a higher chance of death.
Although having an apple shape is not nearly as healthy as eating an apple daily, it may keep the doctor away. Now, Japanese researchers have demonstrated that if they catch COVID-19, people who carry their weight in their bellies may be at greater risk of poor outcomes. Researchers from Tokyo Medical and Dental University (TMDU) discovered in a study that was published last month in Proceedings of the National Academy of Sciences that having too much belly fat is linked to more inflammation and death in Japanese COVID-19 patients. A dangerous condition known as a "cytokine storm" occurs in some
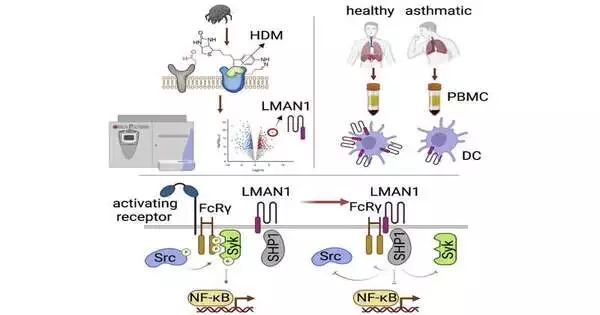
The body's inflammatory cytokines, which react to allergens and cause excessive mucus production, wheezing, and difficulty breathing, have been the primary focus of allergy and asthma research and treatment for many years. Drugs that are frequently prescribed to patients, such as omalizumab, dupilumab, mepolizumab, and reslizumab, lower or block the various cytokines and antibodies that are responsible for the asthmatic response. However, their effects only take effect once a patient's airway inflammation is well established. Dr. Tigno-Aranjuez sought a novel strategy for preventing allergen receptors from reacting in the first place. As a result, she used a method known as
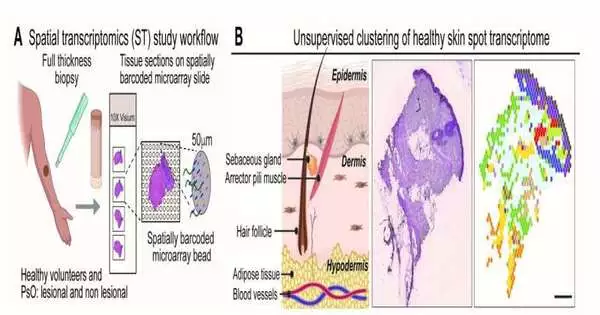
A new study demonstrates that the activity of key cells and signaling pathways distinguishes mild and severe psoriasis from the reddish, flaky lesions that occur on the skin of people with the disease. The study, which was led by researchers at NYU Grossman School of Medicine, mapped hidden characteristics of inflammation and compared them in cases of psoriatic disease that got worse. The team's findings may help explain how small areas of skin inflammation can affect multiple body parts. According to the findings, psoriatic arthritis, or joint inflammation, affects up to one fifth of people with the skin disease. According
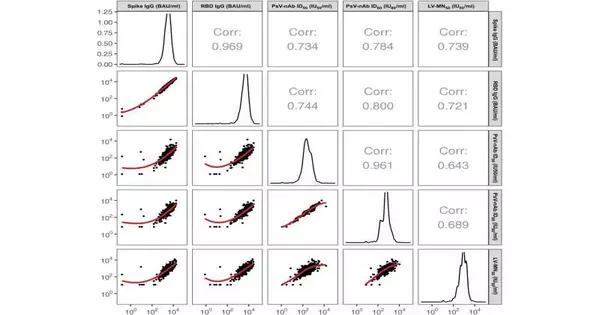
A new study sheds light on antibody measurements that can assist in predicting the Moderna mRNA vaccine's COVID-19 protective capabilities. In order to find potential correlates of protection—CoPs—the measurement of immunological markers that are associated with the level of vaccine protection, such as the quantity of antibodies—the researchers looked at data from a phase 3 clinical trial as well as data from the laboratory. A CoP is an important test that shows how well a particular vaccine protects people from infection. Another way to look at it is that a CoP is a sign in the immune system that, once