A new study on regenerative health reveals the primary beneficial conveyance of mRNA to placental cells to treat toxemia at its root.
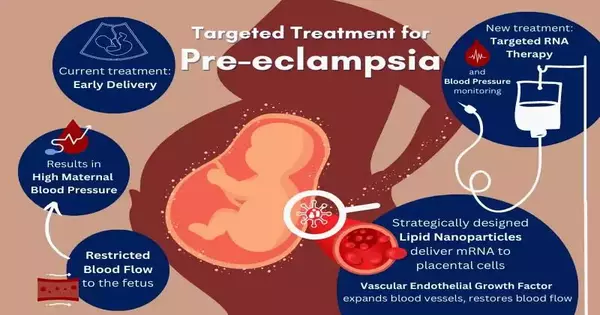
Toxemia is a main cause of stillbirths and rashness around the world, happening in 3–8% of pregnancies. High maternal circulatory strain causes a lack of vasodilation in the placenta, limiting the blood flow from the mother to the hatchling.
At present, a medical service plan for somebody with toxemia includes dietary and developmental changes, continuous observation, pulsing the board, and, in some cases, early conveyance of the child. These guidelines of care address side effects of the condition, not the main driver, and further propagate a wellbeing imbalance.
Presently, College of Pennsylvania engineers are tending to this longstanding hole in conceptive medical services with designated RNA treatment.
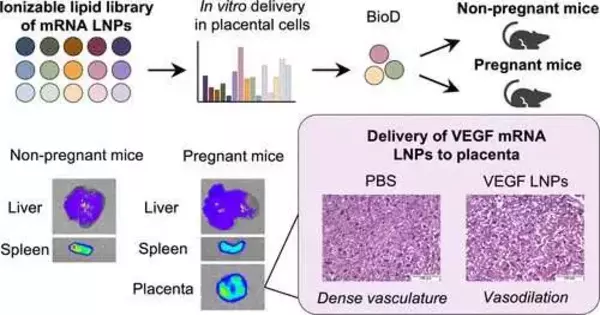
“Our first step was to compile a library of LNPs utilizing the knowledge we gained from our research on LNP delivery to the liver. It turns out that the liver and placenta are quite similar. Both have numerous blood veins and receive a lot of blood flow.”
Kelsey Swingle, Ph.D. student in the Mitchell Lab and lead author.
The coronavirus immunizations showed how lipid nanoparticles (LNPs) proficiently convey mRNA to target cells. LNPs are paving the way for a variety of RNA treatments aimed at treating the underlying causes of disease and illness.Notwithstanding, drug improvement and medical services have reliably ignored a piece of the population that needs designated care the most—pregnant individuals and their children.
Michael Mitchell, J. Peter, and Geri Skirkanich, right-hand teachers of advancement in bioengineering, and Kelsey Swingle, Ph.D. understudy in the Mitchell Lab and lead creator, depict their advancement of a LNP with the capacity to target and convey mRNA to trophoblasts, endothelial cells, and safe cells in the placenta in one of the primary studies of its kind, distributed in the Journal of the American Substance Society.
When these cells get the mRNA, they make vascular endothelial development factor (VEGF), a protein that grows the veins in the placenta to decrease the mother’s circulatory strain and restore a satisfactory course for the baby. The specialists’ effective preliminary tests in mice might prompt promising medicines for toxemia in people.
“Current medical services for women with toxemia are inadequate,” Swingle says.”Ordinarily, the main thing specialists have had the option to do is plan for an early delivery, bringing about untimely births that accompany related difficulties.” “This approach is just deteriorating the wellbeing of moms and their children where untimely consideration is restricted.”
Swingle spearheaded this concentration on LNP-aided RNA treatments for pregnant ladies and their infants. This is whenever LNP-first assisted mRNA conveyance to the placenta has been demonstrated.
“With no prior exploration to draw on, our most memorable test was determining which LNPs would truly venture out and focus on the placenta,” Swingle says.”We began by making a library of LNPs, utilizing our insight from the work we did on LNP conveyance to the liver. It turns out that the liver and the placenta are quite comparable. “The two of them get high blood flow and contain complex trees of veins.”
By matching a pregnant individual’s regular blood stream to the belly with an exceptionally unambiguous ionizable lipid in the LNP, the exploration group had the option to target and convey VEGF to placental cells in pregnant mice through a basic tail vein infusion.
“The coronavirus immunizations were directed as intramuscular infusions, a jolt,” says Swingle. “This treatment would be directed intravenously. That implies a pregnant lady would have the option of being dealt with through a basic, harmless, and torment-free IV drip.
Pregnant women were excluded from clinical trials for coronavirus immunizations, leaving many questions about how to protect their own and their children’s health.This oversight isn’t new. Most of the medications available have not been tried in pregnant women, and issues during pregnancy are ordinarily untreatable before birth.
Swingle was inspired by the treatment described in the notable review because it improves the health of women.
“I was moved to explore designated treatments for maternal and fetal wellbeing in the spring of 2021 when individuals were settling on conclusions about getting the coronavirus antibody and pregnant ladies had inquiries regarding security that we were unable to reply to,” she says. “On account of toxemia, many children are conceived early, bringing about hindered or unusual development and a physiological turn of events.” A treatment that addresses the issue at its root would result in a higher quality of life and wellbeing for both the child and the mother in the long run.”One way I can support women’s health is to attend to this examination hole.”
The new way to deal with LNP advancement for RNA treatments is opening new entryways for hard-to-treat illnesses. The ongoing review is only one illustration of where this work is going.
“While specialists have been working on instruments and the development of medications into cells, there isn’t much out there on how treatments can be designated to treat the underlying drivers of infections and conditions, particularly during pregnancy,” Mitchell says. “We currently have another LNP stage and can fit and play different RNA therapeutics to foster fruitful treatments for the majority of pregnancy conditions.” This work is jumping off that stage, and we are eager to make the following strides.
More information: Kelsey L. Swingle et al, Ionizable Lipid Nanoparticles for In Vivo mRNA Delivery to the Placenta during Pregnancy, Journal of the American Chemical Society (2023). DOI: 10.1021/jacs.2c12893