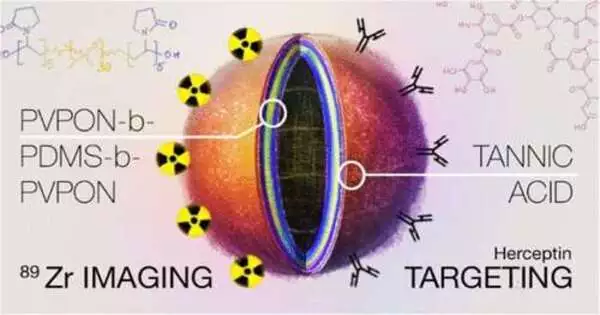
A perfect nanovesicle for fighting cancer would have three functions: 1) a precision-targeting molecule to preferentially bind it to surface markers on cancer cells, 2) a strongly bound radionuclide signal to locate the vesicles in the body, and 3) the capacity to carry and release a drug treatment, such as chemotherapy, at the cancer tumor.
It would also satisfy two additional requirements, including having an easy and straightforward manufacturing process and being biocompatible and biodegradable in the body.
A small polymersome that appears to overcome these obstacles in preliminary preclinical experiments has now been described by a team from the University of Alabama at Birmingham. Each polymersome is hollow and has a thin wall, but the coating on the polymersome represents a development.
Tannic acid, or TA, is adsorbed onto the surface of the 60-nanometer triblock copolymer polymersomes through hydrogen bonding. According to Eugenia Kharlampieva, Ph.D., this TA is then capable of binding a monoclonal antibody-targeting molecule and zirconium radionuclide, or Zr, without the need to create specialized linkers like chelators. D. as well as Suzanne E. Liapi, Ph. D., leaders of the UAB group. They have their research in the book, Biomacromolecules.
“To the best of our knowledge, our work is the first example of a chelator-free-radiiolabeled polymersome capable of a long-term multiday PET imaging study in vivo,”
Suzanne E. Lapi, Ph.D., leaders of the UAB team.
According to Kharlampieva, a distinguished researcher, “in this study, we have developed a straightforward method for a chelator-free modification of the PVPON5-PDMS30-PVPON5 triblock copolymer nanovesicles, about 60 to 80 nanometers in diameter, with a layer of polyphenol that can be used to anchor 89Zr radiotracer or other active metal ions for molecular imaging, as well as HER2-targeting. Within the triblock copolymer, PVPON5 is a brief, five-monomer hydrophilic polymer block, and PDMS30 is a longer, 30-monomer hydrophobic polymer block.
The mortality rate from breast cancer, one of the most prevalent cancers, is still high on a global scale. Current treatments include therapeutic antibodies or systemic drugs, but these are frequently linked to heart dysfunction and damage. Drug activity might be effective while posing fewer toxicity risks with image-guided drug delivery to a solid tumor.
According to Lapi, director of the UAB Cyclotron Facility and professor in the UAB Department of Radiology, “to the best of our knowledge, our work represents the first example of a chelator-free, radiolabeled polymersome capable of a long-term, multiday PET imaging study in vivo.”. The radiolabeling strategy created here may be able to provide stable binding of a variety of isotopes without radiometal leaching from the vesicle membrane in vivo. Notably, this strategy combines the inherent benefits of a polyphenolic polymersome membrane with the advantage of rapidly anchoring ligands that target breast cancer cells.
In the study, TA on the polymersome bound the trastuzumab monoclonal antibody, or Tmab, through ionic and hydrogen bonding as well as nonspecific ionic pairing to the 89Zr4 radionuclide. PET scans in healthy mice showed excellent retention of the 89Zr for up to seven days.
As opposed to currently available covalent methods, the noncovalent Tmab anchoring to the polymersome membrane can be extremely advantageous for nanoparticle modification, according to Kharlampieva. It enables the simple and quick integration of a wide variety of targeting proteins. “Given that these polymersomes can encapsulate and release anticancer therapeutics, they can be further developed as precision-targeted therapeutic carriers for advancing human health through highly efficient drug-delivery techniques.”.
Radiolabeling yields of 97 percent were obtained after incubating the TA-polymersomes in a solution of 89Zr-oxalate for one hour; these yields persisted for one, three, and seven days. In vitro incubations with two lines of cancer cells for up to four days did not cause any cytotoxicity in the labeled polymersomes. Furthermore, binding of 89Zr to polymersomes with Tmab already attached had high yields (97 percent) and stability for seven days. The UAB scientists claim that these binding yields are high enough for clinical use.
The stable retention of the 89Zr on the TA-polymersomes was then indirectly shown in mice.
Because the zirconium is chelated with phosphate moieties in the bone, the biodistribution of free 89Zr radiotracer has previously been shown to localize primarily in the spine and femurs of animals. When free 89Zr was injected into mice, the UAB researchers discovered that, after 24 hours, a PET scan showed that nearly all of it was located in the femur bones. When mice were given injections of 89Zr-TA-polymersomes, a significantly different biodistribution was observed. The bones contained very little radioactivity, while the liver and spleen contained almost all of it. At that point, nanomaterials larger than 6 to 8 nanometers represent the known anticipated clearance of nanovesicles through the mononuclear phagocyte system.
The stark contrast between the biodistribution of free 89Zr and the metal radiotracer-labeled vesicle that was observed, according to Lapi, is significant because it shows how easily the polymeric nanocarrier can be tracked in vivo.
It is further proof of the tight retention of the 89Zr on the TA-polymersomes that the mice’s strong imaging contrast was maintained for seven days.
By differentially binding the nanovesicles to HER2-positive breast cancer cells versus HER2-negative cells in vitro, the 89Zr-Tmab-TA-polymersomes’ capacity to target HER2-positive cancer cells was demonstrated. According to the researchers, additional research is necessary to focus on breast cancer tumors in animals.
Veronika Kozlovskaya, from the UAB Department of Chemistry, and Maxwell Ducharme, from the UAB Department of Radiology, are the study’s co-first authors. Their title is “Direct radiolabeling of trastuzumab-targeting triblock copolymer vesicles with 89Zr for positron emission tomography imaging.”.
Along with Kharlampieva, Lapi, Kozlovskaya, and Durcharme, the study also includes Volkan Tekin from the UAB Department of Radiology, Maksim Dolmat, and James M. Omweri from the Chemistry Department at UAB.
More information: Veronika Kozlovskaya et al, Direct Radiolabeling of Trastuzumab-Targeting Triblock Copolymer Vesicles with 89Zr for Positron Emission Tomography Imaging, Biomacromolecules (2023). DOI: 10.1021/acs.biomac.2c01539