A new examination has shown a relationship between low-quality sleep—uunder seven hours—aand Alzheimer’s disease-related pathology in individuals without mental debilitation. The concentrate, created by a global group driven by the Pasqual Maragall Establishment research focus, the Barcelonaeta Cerebrum Exploration Center (BBRC), along with scientists from the College of Bristol and North Bristol NHS Trust, was distributed in the diary Mind Correspondences on Nov. 3.
The aftereffects of the examination, part of the European Counteraction of Alzheimer’s Dementia Longitudinal Companion Study (EPAD LCS), demonstrate that unfortunate rest quality is connected with an expansion in the pathology of Alzheimer’s illness. This finding is pertinent to helping characterize future treatments so they can be focused on at the right stage of the illness.
A cross-sectional investigation of rest quality
Rest anomalies are normal in Alzheimer’s disease, and rest quality can be impacted from the get-go in the preclinical phase of the illness, in any event, when no different side effects are capable. Figuring out how and when lack of sleep adds to Alzheimer’s disease movement is significant for the planning and execution of future treatments.
Laura Stankeviciute, a predoctoral specialist at the BBRC and one of the fundamental writers of the review, said, “The epidemiological and exploratory information accessible to date previously proposed that rest irregularities add to the gamble of Alzheimer’s disease.”
“Through these studies, we were able to investigate relationships between the primary biomarkers of Alzheimer’s disease and various sleep quality measures, including as total score, duration, efficiency, and change.”
Dr. Oriol Grau, Head of the Clinical Research Group
“Notwithstanding, past investigations had limits because of the absence of biomarkers of Alzheimer’s infection, since they had a non-cross-sectional plan, or in light of the small size of the examples of members.” This is the main review to incorporate these elements.
The biggest associate to date for an examination of rest quality and productivity
Utilizing information from the biggest companion to date, the EPAD LCS, specialists had the option to approve the speculation that lack of sleep is related to cerebrospinal fluid (CSF) biomarkers of Alzheimer’s disease cross-sectionally and predicts future expansions in illness in individuals without recognizable side effects of Alzheimer’s disease at benchmark.
The BBRC group, as a team with scientists from the College of Bristol, broke down information from 1,168 grown-ups north of 50 years old, remembering biomarkers of Alzheimer’s disease for cerebrospinal fluid, mental execution, and rest quality. To quantify the last option, they utilized the Pittsburgh Rest Quality Index (PSQI) survey.
Dr. Liz Coulthard, academic partner in dementia and nervous system science at the College of Bristol and nervous system specialist at the North Bristol NHS Trust, added, “Rest is an undiscovered chance to assist with forestalling Alzheimer’s and advance mental wellbeing.” Our patients were incredibly dedicated to the EPAD review, finishing many tests, including lumbar cuts for research. Their important information, joined with different locales around Europe, has now prompted a superior comprehension of the connections between rest and Alzheimer’s.
Dr. Oriol Grau, Top of the Clinical Exploration Gathering and Hazard Elements for Neurodegenerative Infections of the BBRC, made sense of, “Through these investigations, we have had the option to concentrate on the relationship between the primary biomarkers of Alzheimer’s sickness and various proportions of rest quality, like its complete score, length, productivity, and change.”
By breaking down cerebrospinal liquid examples from 332 members taken at standard and after a normal time of 1.5 years, scientists evaluated the impact of benchmark rest quality on change in biomarkers of Alzheimer’s disease over the long haul.
Preventive practices to further develop quality rest
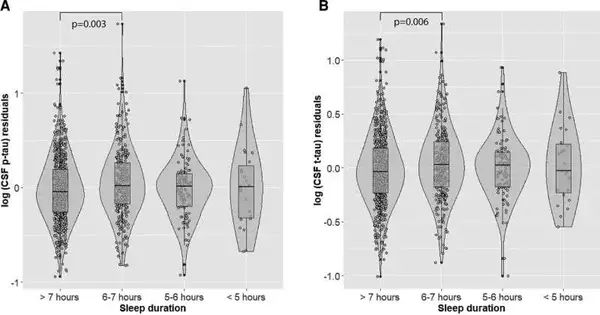
Cross-sectional examinations uncovered that the unfortunate rest quality is altogether connected with expanded t-tau protein in cerebrospinal fluid. Among different discoveries, it was shown that a brief length of rest, under seven hours, is related to higher upsides of p-tau and t-tau, key biomarkers to gauge Alzheimer’s disease in the preclinical period of the illness. Moreover, longitudinal examinations showed that more prominent rest aggravations were related to a decline in the A42 biomarker over the long haul.
This study shows that members’ unfortunate rest quality is related to more prominent Alzheimer’s disease-related pathology in people without a mental disability.
Laura Stankeviciute added, “Our outcomes further reinforce the speculation that rest disturbance might imply a liability factor for Alzheimer’s illness.” “Consequently, future examination is expected to test the adequacy of preventive practices intended to further develop rest in the presymptomatic phases of the illness and decrease the pathology of Alzheimer’s disease.”
More information: Jonathan Blackman et al, Cross-sectional and longitudinal association of sleep and Alzheimer biomarkers in cognitively unimpaired adults, Brain Communications (2022). DOI: 10.1093/braincomms/fcac257
Journal information: Brain Communications