A new study demonstrates that the activity of key cells and signaling pathways distinguishes mild and severe psoriasis from the reddish, flaky lesions that occur on the skin of people with the disease.
The study, which was led by researchers at NYU Grossman School of Medicine, mapped hidden characteristics of inflammation and compared them in cases of psoriatic disease that got worse. The team’s findings may help explain how small areas of skin inflammation can affect multiple body parts. According to the findings, psoriatic arthritis, or joint inflammation, affects up to one fifth of people with the skin disease. According to them, the findings of the study may also provide explanations for how psoriasis can lead to other conditions like type 2 diabetes, heart disease, and inflammatory bowel disease.
New analyses, which were published online June 2 in the journal Science Immunology, revealed that in more severe cases of psoriasis, the location of clusters of cells known as fibroblasts, which are key regulators of inflammation, and macrophages, a type of white blood cell, varied and was more prevalent in the upper layers of the skin.
“Our initial aim was to find quantifiable molecular signals that could tell us who is more likely to develop severe psoriasis, as well as who is more likely to develop related disorders that frequently accompany psoriasis, such as arthritis and cardiovascular disease,”
Study co-senior investigator Jose Scher, MD.
Further, the examination group found that in skin tests from patients with moderate-to-extreme psoriatic sickness, quality action expanded in multiple dozen sub-atomic pathways attached to digestion and control of lipid levels, factors known to turn out badly in diabetes and cardiovascular illnesses. Even in clear skin that was far from any lesions, this increased gene activity was observed.
Jose Scher, MD, co-senior investigator of the study, stated, “Our initial goal was to find measurable molecular signals that could tell us who is more likely to develop severe psoriasis, as well as who is at higher risk of developing related disorders that frequently accompany psoriasis, such as arthritis and cardiovascular disease.”
“Having found signals with possible fundamental outcomes, we are presently attempting to comprehend what skin irritation can prompt far and wide illness meaning for different organs,” said Scher, the Steere Abramson Academic Administrator of Medication in the Branch of Medication at NYU Langone Wellbeing, where he additionally fills in as overseer of its Psoriatic Joint Pain Community and the Judith and Stewart Colton Place for Autoimmunity.
Senior investigator Shruti Naik, Ph.D., who works in the Ronald O. Perelman Department of Dermatology at NYU Langone, said, “Our study serves as a valuable resource for the scientific community, offering the most comprehensive archive of cellular and molecular features involved in both diseased and healthy skin.”
Psoriatic arthritis is thought to affect over 8 million people in the United States and 125 million people worldwide. Both men and women are affected by the condition.
According to Scher, the new study was intended to go beyond the current diagnostic methods, which instead of focusing on the visible symptoms of skin lesions, examine their invisible systemic and molecular effects. Although many of the available treatments, such as steroids and immunosuppressive medications, alleviate symptoms and inflammation, they do not address the disease’s underlying causes.
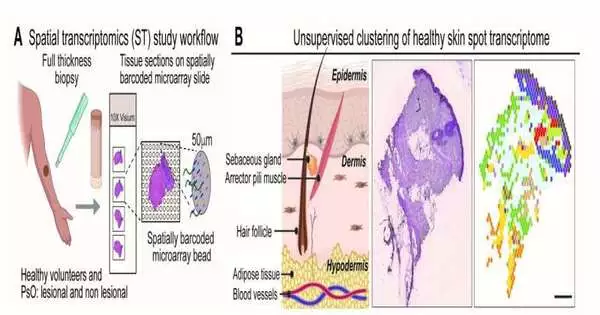
The new research made use of spatial transcriptomics, a method that meticulously records the molecular and cellular interactions that take place in a particular tissue. The intact skin samples of 11 men and women with mild to severe psoriatic disease and three healthy adults without the condition were analyzed by the researchers. They claim that spatial transcriptomics is more effective than other commonly used methods for tracking individual cells because it creates a comprehensive image-based map of where cells are located in tissues and what other cells they communicate with.
According to Naik, the team intends to utilize their most recent analysis to determine the biological mechanisms underlying skin inflammation in one region and its effects on skin or other organs in another region. In order to learn how and why some patients respond differently to the same anti-inflammatory medications and how the disease clears up on its own, additional research is planned on larger groups of patients as well as on skin with and without lesions from the same patients.
For the benefit of researchers worldwide, study co-lead investigator and bioinformatician Ikjot Sidhu has archived its spatial transcriptomics analysis online at https://zenodo.org/record/7813973 and https://zenodo.org/record/7562864 .