Northwestern College scientists have fostered the main material science-based measurement to foresee whether an individual could some time or another experience an aortic aneurysm, a dangerous condition that frequently causes no side effects until it cracks.
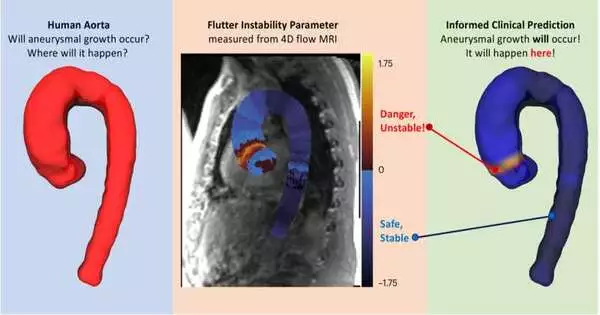
By measuring subtle “fluttering” in a patient’s blood vessel, the researchers in the new study predicted abnormal aortic growth. As blood courses through the aorta, it can cause the vessel wall to shudder, like how a pennant swells in the breeze. According to the findings of the researchers, unstable flutter is highly predictive of future abnormal growth and potential rupture, whereas stable flow predicts normal, natural growth.
Called the “shudder insecurity boundary” (FIP), the new measurement anticipated future aneurysms with 98% precision on average three years after the FIP was first estimated. To compute a customized FIP, patients just need a solitary 4D stream attractive reverberation imaging (X-ray) check.
Utilizing clinically quantifiable, prescient measurement, doctors could endorse drugs to high-gamble with patients to intercede and possibly keep the aorta from enlarging to a hazardous size.
The study was published in Nature Biomedical Engineering on December 11 of this year.
“Aortic aneurysms are casually alluded to as ‘quiet executioners’ since they frequently go undetected until horrendous analyzation or cracking happens,” said Northwestern’s Neelesh A. Patankar, senior creator of the review. “The essential material science driving aneurysms has been obscured. Therefore, there is no clinically accepted method for predicting them. Presently, we have shown the viability of a material science-based metric that predicts future development. This could be groundbreaking in anticipating heart pathologies.”
Patankar, a specialist on liquid elements, is a teacher of mechanical design at Northwestern’s McCormick School of Design. He co-droved the review with Dr. Tom Zhao, who spends significant time in first-standard biomechanics.
Growing risk An aortic aneurysm occurs when the aorta—the body’s largest artery—swells to more than 1.5 times its original size. As it develops, the aorta’s wall debilitates. In the end, the wall turns out to be feeble to the point that it can never again endure the strain of blood moving through it, making the aorta break. Aortic rupture is usually unpredictable and almost always fatal, despite its rarity.
A few noticeable individuals have passed on from aortic aneurysm, including Award Wahl, a games writer who kicked the bucket out of nowhere one year prior at the 2022 FIFA World Cup. Other VIP passes incorporate John Ritter, Lucille Ball, and Albert Einstein.
“A great many people don’t understand they have an aneurysm except if it is coincidentally identified when they get an output for an inconsequential issue,” Patankar said. “Medications to lower cholesterol, heart rate, and blood pressure can be prescribed by doctors if they find them. Assuming that it goes undetected, it can break, which is a devastating occasion.”
“The death rate is close to 100 percent if it ruptures while the person is outside of a hospital,” Zhao added. Critical organs, like the brain, are unable to function as a result of the body’s lack of blood supply.”
Eliminating the mystery
For the current norm of care, doctors gauge the chance of a crack in view of hazard factors (like age or smoking history) and the size of the aorta. Regular imaging scans are used by doctors to track a growing aorta. In the event that the aorta begins to develop excessively fast or becomes too enormous, a patient will frequently go through a careful unite to support the vessel wall, an obtrusive methodology that conveys its own dangers.
“Our aggregate absence of understanding makes it hard to screen for aneurysm movement,” Zhao said. “An aneurysm’s size must be monitored by imaging its location every one to five years, depending on how quickly it grew in the past and whether the patient has any diseases associated with it. Over this’sit back and watch’ period, an aneurysm can lethally burst.”
Play 00:00 00:01 Shut down Settings PIP and play in fullscreen. Watch blood flow through an aorta. Credit: Ethan Johnson/Northwestern College
To eliminate the mystery of anticipating future aneurysms, Patankar, Zhao, and their teammates tried to catch the central material science fundamentals of the issue. They discovered through extensive mathematical work and analyses that issues arise when the fluttering vessel wall changes from stable to unstable. This flimsiness either causes or signals an aneurysm.
“Shuddering is a mechanical mark of future development,” Patankar said.
The researchers combined blood pressure, aorta size, stiffness of the aortic wall, shear stress on the wall, and pulse rate to quantify the transition from stability to instability. The subsequent number (or FIP) describes the specific communication between circulatory strain and wall solidity that, at last, triggers vacillating flimsiness.
“Doctors have known that these elements—circulatory strain, heartbeat recurrence, and aortic size—were involved, yet they didn’t have any idea how to evaluate them,” Patankar said. “It turns out the mix of the elements is what’s significant. A patient could have an unsteady wall, however, an ordinary estimated aorta, so their primary care physician wouldn’t understand there was an issue.”
Shockingly, the analysts found that shakiness will in general emerge when the wall is more adaptable. This finding straightforwardly goes against common sense that aortic solidity is an indication of illness.
Zhao stated, “We show that the patient is more at risk for future growth and rupture when it is less stiff.” This is because the body tries to stiffen the aorta when it reaches a certain size to appear to protect it from future growth. However, the ones that are nonetheless growing are less rigid. The aorta will shudder, assuming the wall is more consistent.”
Approving the measurement
To test the new measurement, the scientists assessed 4D stream X-ray information from 117 patients who went through cardiovascular imaging to screen for coronary illness and from 100 solid workers. In view of this X-ray, the scientists assigned every patient a customized FIP. In this measurement, zero denotes the limit between steady and unsound.
Aortic abnormal growth was unlikely to occur in patients with a FIP below zero. Scientists anticipated that patients with a FIP higher than nothing, notwithstanding, would encounter unusual development and a future burst.
“In laying out the prognostic value of this quantitative measurement for cardiovascular 4D stream X-ray, we can fundamentally work on the benefit of imaging presented as a standard of care to patients with aneurysms,” said Dr. Ethan Johnson, the review’s co-first creator and a postdoctoral individual in cardiovascular imaging at Northwestern College Feinberg Institute of Medication.
At the point when the specialists contrasted these forecasts with follow-up X-rays or doctor analyze, they found their expectations were precise in 98% of the cases. The researchers claim that this metric may even provide a more granular view of heart health on a daily or monthly basis, even though the FIP predicted future growth on average three years after the initial MRI (when the FIP was calculated).
“The time range of one to eight years is the time range in which our clinical information sits,” Zhao said. “Not the all-out time span wherein the FIP is fundamentally powerful.”
Then, Patankar, Zhao, and their group intend to investigate on the off chance that the FIP can give pieces of information into how other heart conditions create. They likewise are examining in the event that patient-explicit FIP can show which avoidance techniques are best in halting aneurysm movement.
The exploration is named “Blood-wall vacillating unsteadiness as a physiomarker of the movement of thoracic aortic aneurysms.”
More information: Tom Y. Zhao et al, Blood–wall fluttering instability as a physiomarker of the progression of thoracic aortic aneurysms, Nature Biomedical Engineering (2023). DOI: 10.1038/s41551-023-01130-1