Plastics are among the most universal artificial materials — we wear them, work with them, play with them, transport products in them, and afterward we toss them into the waste stream. In the end, they may decompose into microscopic particles that enter our food supply and we consume.
These particles, which can be as small as a grain of pollen (microplastics) or as large as a virus (nanoplastics), have entered water supplies, agricultural soil beds, natural food chains, and domestic food chains.
Due to their ubiquitous nature, which makes it difficult to locate populations of unaffected individuals to serve as control groups, and the absence of relevant laboratory models for examining the effects of the particles on cells, knowledge of the effects of ingesting microplastics and nanoplastics has been limited.
In a review distributed in Nanomedicine: Using human intestinal organoids, which are small bundles of tissue made from a mixture of human cells obtained from biopsies and that mimic the complexity of an actual intestinal environment, researchers at Tufts University School of Engineering from the departments of nanotechnology, biology, and medicine have discovered potential inflammatory effects of plastic particles.
“The findings of this study indicate that using human cell organoids could be an effective way to better understand the potential toxicity of microplastics and nanoplastics, as well as environmental particles in general,”
David Kaplan, Stern Family Professor of Engineering at Tufts .
Notably, the researchers discovered that the secretion of inflammatory molecules linked to human inflammatory bowel disease (IBD) was triggered by higher concentrations of plastic particles.
According to previous clinical studies, plastics have accumulated in a variety of living organisms’ tissues, including the digestive tract, blood, liver, pancreas, heart, and even the brain. The intestine is most likely the first entry point. Concentrates on rodents and different creatures have found that while microplastics and nanoplastics may amass in the digestive system and different tissues, there are clashing outcomes on poisonous impacts or aggravation, which might rely upon molecule size, length of openness, and previous circumstances. Because the outcomes of animal studies do not always correspond to those of human studies, it is still up for debate whether there are any toxicological effects on humans.
“We realize that particulate plastic is everywhere in the climate, and it has been tracked down in human digestion tracts and different tissues, similar to blood, and, surprisingly, in the cerebrum and placenta,” said Ying Chen, research right hand teacher in biomedical design at Tufts College and co-lead creator of the review. “With the help of organoids, we are able to investigate in depth the mechanisms of absorption and potential disease pathways, which may help us make sense of the inconsistent findings in the prior research and provide a more precise tissue model for the potential effects of plastic particles on humans.
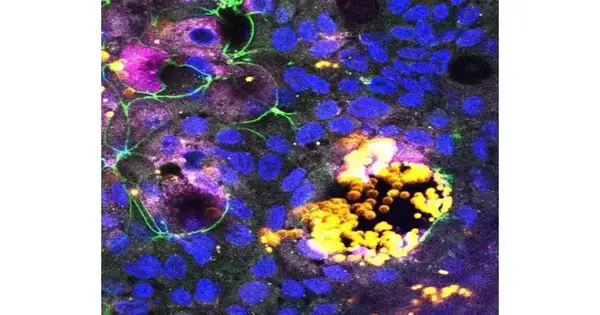
Chen and her colleagues started with organoid stem cells and coaxed them to differentiate into the various cells that are found in the native intestinal wall in order to create a physiologically relevant intestinal model. The goal was to achieve a cell ratio that was comparable to that of the intestine but was grown in a flat layer. The cells play a variety of important roles, including absorbing nutrients, producing hormones, secreting mucus, and responding to inflammatory and other immune responses.
“It’s a huge move forward from less difficult cell models that frequently included only one or a couple of cell types, some of which were gotten from malignant growth cells that probably won’t show normal reactions,” said Chen. They had the option to change the blend of cells in the digestive tract, like the organoid layer, to perceive what it meant for the reaction to plastic particles, which were extraordinarily adjusted to shine fluorescently for simple following.
Various cells were found to ingest various sizes of particles. Epithelial cells that typically line the digestive system would assimilate the smallest nanoparticles, while microfold or “M” cells would retain and ship bigger microparticles into the gastrointestinal tissue. Additionally, the researchers discovered that only M cells were present and that higher concentrations of plastic particles caused damage to the model intestinal lining. Lesions in the intestine could result from damage to the cell layer.
Strikingly, the scientists likewise saw that higher centralizations of plastic nanoparticles set off the organoid layer to deliver provocative cytokines — particles that are a piece of the typical resistant reaction yet may connect with illnesses including inflammatory bowel disease (IBD) when they are set wobbly. Additionally, the presence of M cells was necessary for this effect to occur, indicating that these cells are crucial in preventing plastic microparticles from causing damage to the intestine. Ying stated that additional research will be required to clarify the effect of plastic particle concentration, chemistry, and surface characteristics on M cell functions.
David Kaplan, a pioneer in tissue engineering and the development of laboratory test models that mimic real biological tissues, stated, “The results in this study suggest that using human cell organoids could be an effective means to better understand the potential toxicity of microplastics and nanoplastics, as well as environmental particles in general.” Kaplan is a Stern Family Professor of Engineering at Tufts. The potential impact of the studies is amplified by the fact that these tiny particles can also serve as environmental sinks or carriers for chemicals and other contaminants.”
“In fact, organoids can be grown to model many other human organs, including the stomach, kidneys, heart, pancreas, liver, and brain,” Kaplan continues, “which could enable us to explore the effects of environmental contaminants throughout the body.” Organoids can also be grown to model the brain and pancreas.
More information: Ying Chen et al, Biological effects of polystyrene micro- and nano-plastics on human intestinal organoid-derived epithelial tissue models without and with M cells, Nanomedicine: Nanotechnology, Biology and Medicine (2023). DOI: 10.1016/j.nano.2023.102680