Like the Roadrunner outmaneuvering Wile E. Coyote, SARS-CoV-2 (the irresistible infection liable for Coronavirus) continues changing, producing new variations that can slip from the hold of a thoroughly prepared safe framework or a very well targeted medication or immunization.
Presently, Stanford Medication researchers have figured out how to saturate safe particles once thought futile with the capacity to place SARS-CoV-2 in a restorative headlock it can’t wriggle out of. Their strategy is outlined in a paper distributed Sept. 8 in Nature Compound Science. The review was led by researcher and vaccinologist Peter Kim, Ph.D.
Two things about the review stick out. To begin with, in spite of the fact that it’s not prepared at this point for use in people, it’s a strong move toward the improvement of extensively compelling medications that don’t quit working on the grounds that a terrible infection has concocted another stunt. Furthermore, second, a critical part of the new treatment was a particle that had been regularly getting thrown in the rubbish.
“You go through all the work of generating these monoclonal antibodies, guiding them through clinical trials, establishing manufacturing operations, and obtaining FDA emergency use authorization. The virus then mutates months later, rendering the monoclonal antibody useless.”
Biologist and vaccinologist Peter Kim, Ph.D.
To completely see the value in Kim’s group’s disclosure, we should step back and inquire: what precisely happens when an infection contaminates our bodies? Also, what does the resistant framework do about it?
The fundamentals of disease
To cause contamination, an infection should initially get inside a cell. Cells’ external films are ordinarily hard to infiltrate without a unique pass. In any case, these little protected wafers have figured how to prod open a lock on the cell’s surface, move in, commandeer the cell’s replication hardware, make a bazillion duplicates of themselves and break out to spread to different cells.
The lock SARS-CoV-2 knows how to pick is ACE2, that shows up on the outer layer of cells in the throat, lungs, heart, kidney, digestion tracts and vein linings. ACE2 is popular for, in addition to other things, assisting keep our blood with compelling low. However, SARS-CoV-2 doesn’t mind at all how ACE2 makes ends meet. Any phone bearing ACE2 is helpless against SARS-CoV-2 contamination.
Our resistant framework has approaches to managing such gatecrashers. After perceiving a microbe’s presence, B cells, which assist in making up our insusceptible framework, siphon out an expansive collection of antibodies focused on the intruder. These are particles interestingly fitted to glom onto microorganisms like matching jigsaw-unique pieces and—when they glom onto the perfect spots and the fit is great—putting them down and out.
Antibodies that succeed in taking hold of some element pivotal to the microbe’s cell safe-breaking achievement are announced to be “killing”: they keep the microorganism from contaminating cells. All of these killing antibodies can then be made into drugs.
For example, patients hospitalized with coronavirus frequently get a portion of monoclonal antibodies: different duplicates of the equivalent effectively kill immunizer. The difficulty is, SARS-CoV-2 is capable of tweaking the states of its weak elements by transforming, so a once-killing monoclonal neutralizer loses its hold and can never again suppress the new variation. The coronavirus pandemic has been a motorcade of an endless series of insusceptible slick people.
Enhanced counter-acting agent
“It’s whack-a-mole,” said Kim, who spent a piece of his career working in the drug business. “You go through all that difficulty of fostering these monoclonal antibodies, shepherding them through clinical preliminaries, setting up assembling activities and getting crisis use approval from the FDA. Then, at that point, months after the fact, the infection transforms and the monoclonal immune response is horrible no longer.
Of the in excess of about six SARS-CoV-2-focusing on monoclonal antibodies that have gotten crisis use approval, only one is still being used.
In any case, Kim’s lab has a beefed up immunizer that might take on any and all individuals.
Every one of the monoclonal antibodies the FDA has supported up until this point stick to SARS-CoV-2’s receptor-restricting area, or RBD. That is the “business end” of the infection’s scandalous spike protein, the viral projection that fiddles with ACE2 to acquire permission to cells. By veering off new variations with changed RBDs, the infection continues to shake off progressive monoclonal antibodies’ hold.
However, the SARS-CoV-2 spike protein contains different locales that are, overall, perpetual. These locales are supposed to be profoundly developmentally rationed, meaning they haven’t changed over the long run, even among viral strains that contrast with somewhere else.
All in all, why not concoct a monoclonal immune response that pursues one of those preserved districts? Couldn’t that tackle the slick person?
Indeed, said Kim, who is the Virginia and D. K. Ludwig Teacher in Natural Chemistry. Yet, up until this point, no one has tracked down an immunizer to a preserved district on SARS-CoV-2 that is not a weakling. Overall, it appears that these antibodies are not powerful killing antibodies — they cling to the infection and simply stay there, not preventing it from contaminating cells.
No more stumbling
Kim credits Payton Weidenbacher, Ph.D., a previous alumni understudy in his lab, with a glimmer of creativity that ignited the coming of what they’ve called “ReconnAbs” (another way to say “receptor-obstructing preserved non-killing antibodies”).
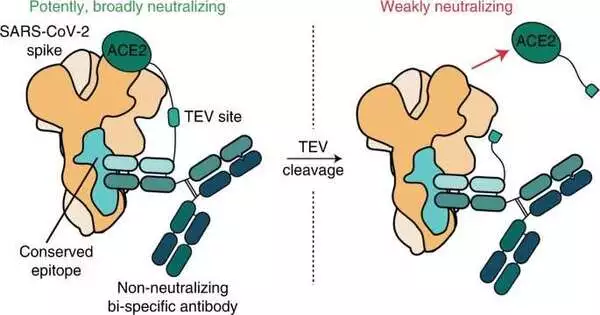
Weidenbacher’s thought: take another particle that could kill SARS-CoV-2 and bind it to one of these weak yet tenacious antibodies that ties to a very much preserved site on the viral spike protein.
“Bunches of different specialists were simply tossing these antibodies in the trash bucket, as were we,” said Weidenbacher.
They found a neutralizer that designated a piece of SARS-CoV2’s spike protein that never appears to change, regardless of what new variation springs up. Involving an adaptable protein scrap as a chain, they fastened this immunizer to the piece of ACE2 that sticks out from the cell surface — the part the infection locks onto.
“It’s absolutely impossible that SARS-CoV-2 can change right out of its reliance on ACE2,” Weidenbacher said.
In a lab dish, the fasted development was shown to be capable of preventing SARS-CoV-2 disease in human cells that are normally susceptible to infection.It’s chipped away at all the SARS-CoV-2 strains tried up through BA.2.
The following stage is to test ReconnAbs on creatures.
Looking past the ongoing pandemic, Kim imagines ReconnAbs filling in as a particular blend and-match “parts unit” that could rapidly be set in motion when the following pandemic hits to slow down the infection every step of the way while anticipating the expected improvement of far superior medications.
Such a unit would contain three sections: antibodies known to stick firmly to unequivocally moderated locales of whatever very concentrated infection (a COVID or flu infection, for instance) goes along; whatever phone surface “lock” that infection knows how to pick to get inside our phones; and a little rope to snare them together.
“It was a stroke of innovativeness,” Kim said. “Payton allegorically ventured into the trash bucket, took out these lemons and transformed them into lemonade.”
More information: Payton A.-B. Weidenbacher et al, Converting non-neutralizing SARS-CoV-2 antibodies into broad-spectrum inhibitors, Nature Chemical Biology (2022). DOI: 10.1038/s41589-022-01140-1
Journal information: Nature Chemical Biology