Researchers at the University of Michigan Rogel Cancer Center were hopeful when they recognized a little particle that impeded a critical pathway in mind growth. Yet, there was an issue: how to help the inhibitor through the circulatory system and into the mind to arrive at the cancer.
In a joint effort with numerous labs, the groups created a nanoparticle to contain the inhibitor, and the outcomes were far better than anticipated.
Not in the least did the nanoparticles convey the inhibitor to the growth in mouse models, where the medication effectively turned on the resistant framework to dispense with the disease. However, the cycle set off safe memory, so a once again introduced cancer was likewise killed — a sign that this potential new methodology couldn’t treat mind growth yet forestall or defer repeats.
“Nobody was able to get this chemical into the brain. It’s a great accomplishment. Glioma patient outcomes have not improved in the last 30 years.”
Maria G. Castro, Ph.D., R.C. Schneider Collegiate Professor of Neurosurgery at Michigan Medicine
“Nobody could get this atom into the cerebrum. It’s actually an immense achievement. Results for patients with glioma have not improved throughout the previous 30 years, “said Maria G. Castro, Ph.D., R.C. Schneider Collegiate Professor of Neurosurgery at Michigan Medicine. Castro is the senior creator of the review, which was published in ACS Nano.
“In spite of the endurance acquired in numerous malignant growth types, glioma remains determinedly testing, with just 5% of patients living five years after their conclusion,” said concentrate on creator Pedro R. Lowenstein, M.D., Ph.D., Richard C. Schneider Collegiate Professor of Neurosurgery at Michigan Medicine.
Gliomas are frequently impervious to customary treatments, and the climate inside the cancer stifles the insusceptible framework, rendering new resistant-based treatments inadequate. Add to that the test of passing the blood cerebrum hindrance, and it turns out to be much harder to convey powerful medicines to these growths.
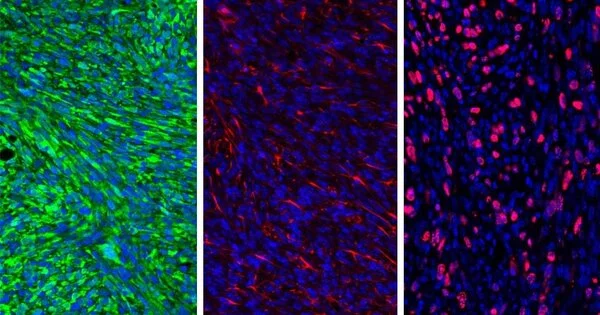
The Castro-Lowenstein lab saw an open door. The little particle inhibitor AMD3100 was created to hinder the activity of CXCR12, a cytokine delivered by the glioma cells that develops a safeguard around the insusceptible framework, keeping it from starting up to face the attacking cancer. CXCR12 was prevented from restricting with resistant suppressive myeloid cells by AMD3100. By incapacitating these cells, the invulnerable framework stays in salvageable shape and can go after the growth cells.
Regardless, AMD3100 was having difficulty reaching the growth. The medication didn’t travel well through the circulatory system, and it didn’t pass the blood-cerebral boundary, a central question in getting drugs into the mind.
The Castro-Lowenstein lab teamed up with Joerg Lahann, Ph.D., Wolfgang Pauli Collegiate Professor of Chemical Engineering at the U-M College of Engineering, to make protein-based nanoparticles to typify the inhibitor, with the expectation of assisting it with going through the circulatory system.
Castro is likewise associated with Anuska V. Andjelkovic, M.D., Ph.D., teacher of pathology and exploration teacher of neurosurgery at Michigan Medicine, whose examination centers around the blood-cerebrum hindrance. They noticed that glioma cancers make strange veins, slowing down the ordinary blood stream.
The analysts infused AMD3100-stacked nanoparticles into mice with gliomas. On a surface level, the nanoparticles contained a peptide linked to a protein found primarily on cerebrum cancer cells. As the nanoparticles went through the circulation system toward the cancer, they delivered AMD3100, which reestablished the trustworthiness of the veins. The nanoparticles could then arrive at their objective, where they delivered the medication, hence impeding the section of the invulnerable suppressive myeloid cells into the growth mass. This permitted the invulnerable cells to kill the growth and delay its movement.
“In the event that you don’t have a blood stream, nothing will get to your objective.” That is the reason weeds are so savvy. “Yet, AMD3100 reestablishes the pathways, which permits the nanoparticles to arrive at the cancer,” Castro said.
Further examinations in mice and patient cell lines exhibited that coupling the AMD3100 nanoparticle with radiation treatment improved the impact of either the nanoparticle or radiation alone.
Among the mice whose tumors were wiped out, the scientists then once again introduced the cancer, recreating a repeat. With practically no extra treatment, 60% of mice remained disease-free. That’s what this recommends. Similar to an immunization, AMD3100 makes invulnerable memory, empowering the resistant framework to perceive and obliterate the once again introduced cells. While it forestalled a repeat in mice, Castro said it looks good for essentially postponing a repeat in individuals.
“Each glioma repeats.” Glioma treatment actually should have this immunological memory, “Castro said.
Starting tests showed next to zero effect on liver, kidney, or heart capacity and typical blood included in the mice after treatment. The nanoparticle has a comparable base as ones that have been recently tried in people and demonstrated to be protected. Extra security testing is essential prior to moving to a clinical preliminary.
More information: Mahmoud S. Alghamri et al, Systemic Delivery of an Adjuvant CXCR4–CXCL12 Signaling Inhibitor Encapsulated in Synthetic Protein Nanoparticles for Glioma Immunotherapy, ACS Nano (2022). DOI: 10.1021/acsnano.1c07492
Journal information: ACS Nano