Researchers have devised a novel method of evaluating aortic development that may aid clinicians in identifying potentially fatal heart diseases earlier. The approach, known as vascular deformation mapping, detects changes in the thoracic aorta by employing high-resolution CT imaging to determine three-dimensional alterations in the aortic wall. VDM considerably outperformed typical manual rating methods done by experts in the study.
Researchers at Michigan Medicine have discovered a novel method of tracking growth in the body’s main artery, which may aid clinicians in detecting potentially fatal cardiac diseases earlier.
The vascular deformation mapping technique examines changes in the thoracic aorta, which transports blood from the heart to the rest of the body. According to data published in Radiology and Medical Physics, this novel technique employs high-resolution CT imaging to quantify three-dimensional changes in the aorta wall in a way that greatly exceeds current manual rating methods performed by professionals.
“The technique used in this algorithm has been around for a while, but no one has ever used it to see three-dimensional growth of a thoracic aortic aneurysm,” said Nicholas Burris, M.D., the papers’ corresponding author, assistant professor of radiology, and director of aortic imaging at Michigan Medicine. “This is an encouraging step toward having technology that increases measurement precision beyond what human raters can achieve, allowing doctors to have the most accurate picture of a patient’s status.”
Recent breakthroughs in artificial intelligence have generated a lot of interest in AI in regard to automating radiology jobs. It turns out that replacing human radiologists is a difficult endeavor, and a more realistic goal for AI is to speed up workflows and assist radiologists in making object, quantitative measures that are otherwise time-consuming and subjective.
Nicholas Burris
Thoracic aortic aneurysm arises when the biggest segment of the aorta weakens and dilates, increasing the risk of a potentially deadly rupture or dissection. Physicians recommend that roughly 3% of adult patients over the age of 50 with this mainly asymptomatic illness have frequent testing, commonly with CT scans, to evaluate aortic development and determine if surgical correction is required.
Currently, the conventional method for measuring growth is to use human “raters” who line up two photos and draw a line between two spots to determine the change. According to Burris, this procedure is prone to error, and in many cases, clinicians are unable to properly determine if the thoracic aorta is developing, raising ambiguity about the optimal treatments and follow-up plan.
“The clinical problem we confront is that a typical aneurysm in the aorta grows only a fraction of a millimeter per year, and the procedure of manually sketching dimensions that accurate is very difficult to replicate,” he explained. “There is a lot of variation in routine measurements compared to a relatively tiny amount of real aneurysm growth. Basically, you rarely get a confident evaluation of growth, which can make it difficult to identify what the patient’s true risk is and how carefully they need to be followed with recurrent CT scans.”
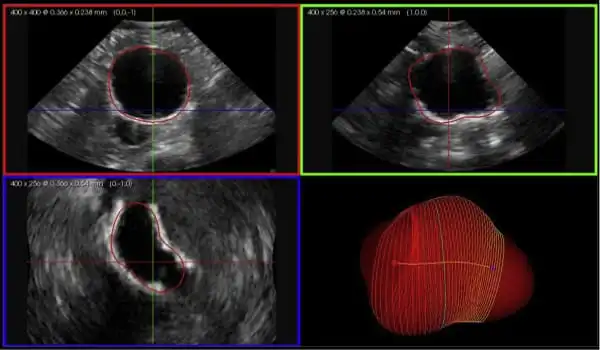
The vascular deformation mapping technique developed by Burris’ team is based on an image analysis technique known as image registration, which essentially aligns the anatomy shown in multiple CT scans by taking any pixel on the first scan and relating its exact position to the pixel on the second scan. When they are all aligned, a three-dimensional color map of the aorta indicates how much and where the thoracic aorta has expanded.
Researchers employed scans from roughly 50 aortic aneurysm patients and 75 reference models with varying aortic wall development for these experiments. They compared the automated algorithm to two expert manual raters and discovered that the vascular deformation mapping surpassed the humans in terms of accuracy and variability in growth metrics. When even the most experienced human analysts had measurements with errors of up to 3 millimeters, vascular deformation mapping reached an accuracy of less than 1 millimeter in all circumstances.
“Recent breakthroughs in artificial intelligence have generated a lot of interest in AI in regard to automating radiology jobs,” said co-author and adjunct research assistant professor of radiology at Michigan Medicine Charles Hatt, Ph.D.
“It turns out that replacing human radiologists is a difficult endeavor, and a more realistic goal for AI is to speed up workflows and assist radiologists in making object, quantitative measures that are otherwise time-consuming and subjective. In this perspective, vascular deformation mapping is an excellent real-world example of how artificial intelligence and quantitative imaging can improve clinical treatment by empowering physicians rather than aiming to replace them.”
While these studies suggest that vascular deformation mapping may be more useful than human rating in determining whether surgery on an aortic aneurysm is essential, researchers say the approach has to be examined further in large groups of patients in a clinic. Fortunately, according to Burris, the vascular deformation mapping approach can be performed on normal CT images of the aorta, making larger research studies easier to conduct.
“This is a completely new way of looking at the growth of aortic aneurysms,” he said. “As research progresses, it may be possible to apply it to a broader range of disorders, such as abdominal aortic aneurysm. Moving from one-dimensional to three-dimensional measurements allows us to detect patterns of aneurysm formation in ways never before achievable, allowing us to ask many new questions and discover how a highly accurate tracking tool like this may be utilized to ultimately enhance patient treatment.”