Examiners from Cedars-Sinai Disease, working in a joint effort with partners in Colorado and the Netherlands, have recognized a particular kind of bladder malignant growth that is probably going to oppose first-line treatment. For some patients with specific subtypes of the disease, their study, which was published today in Science Translational Medicine, may direct clinicians toward more aggressive or targeted therapies, potentially saving lives.
Dan Theodorescu, MD, Ph.D., co-senior author of the study, director of Cedars-Sinai Cancer, and PHASE ONE Distinguished Chair, stated, “These findings provide a potential tool for determining how well patients initially treated for high-risk bladder cancer that isn’t yet muscle-invasive will respond to the most common follow-up therapy.” Clinicians will be able to take advantage of new options being created by precision medicine or make decisions about aggressive surgical treatment that are more informed and timely with this information.”
Every year, more than 80,000 people in the United States are diagnosed with bladder cancer. The majority of these tumors are non-muscle-invasive, meaning they are in the tissue that lines the inside of the bladder and do not involve the bladder muscle. Based on their size, growth rate, and likelihood of spreading, these tumors are categorized as low, intermediate, or high risk.
“Our study’s objective was to discover a new method for identifying these patients before they receive BCG treatment and directing them promptly to more severe treatments that may compromise quality of life but have outstanding long-term results, such as surgical removal of the bladder.”
Dan Theodorescu, MD, Ph.D., co-senior author of the study
The majority of patients with tumors at higher risk receive a course of the immunotherapy Bacillus Calmette-Guérin (BCG) following surgical removal. Only half of patients with high-risk non-muscle invasive bladder cancer benefit from BCG therapy, which is intended to assist the body’s immune system in preventing cancer recurrence.
The remaining 50% of patients experience a recurrence of their cancer within five years, with a 20% chance of developing advanced disease and high mortality rates.
According to Theodorescu, “patients who do not respond have been exposed to unnecessary toxicity from BCG treatment, and their chances of survival may have been compromised due to the delay in receiving more aggressive treatment.” This study’s objective was to discover a novel method for identifying these patients before they receive BCG therapy and directing them immediately to surgical removal of the bladder or other more aggressive therapies, both of which have excellent long-term outcomes but may reduce quality of life.
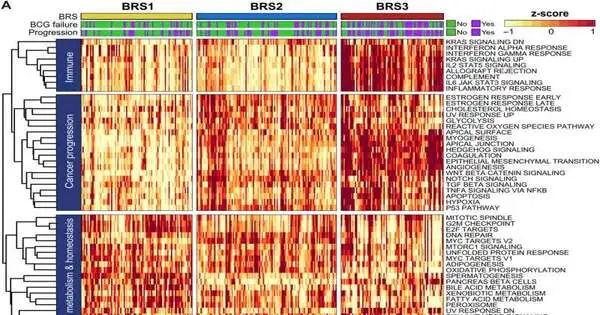
Molecular profiling of non-muscle invasive bladder cancers from 132 patients who had never received BCG treatment and 44 patients whose cancer recurred after receiving BCG treatment was used by the researchers to accomplish this. They matched the clinical outcomes of patients with three distinct subtypes of these tumors to determine whether or not they were associated with cancer recurrence.
One of the subtypes, which examiners call BCG Reaction Subtype 3 (BRS3), was all the more firmly connected with diminished movement-free endurance — meaning less time until the malignant growth repeated — than the other two subtypes. Also, the review’s discoveries showed that BRS3 was the prevailing subtype among patients whose disease repeated after BCG treatment.
Additionally, the researchers were able to demonstrate that BRS3 tumors can be precisely identified by a commercially available test. To further support this finding, a larger follow-up study is currently in progress.
At the 2023 AUA Annual Meeting in April, Theodorescu was presented with a presidential citation by the American Urological Association for “elucidating the underpinnings of urothelial cancer,” which is the most common type of bladder cancer.
According to Theodorescu, “I’m very humbled and honored to be recognized by my clinical peers at the American Urological Association.” This reference to perceiving my logical accomplishments makes a big difference to me.”
When Theodorescu was a graduate student in the 1990s, he first became interested in bladder cancer. Since then, he has worked in the field and has continued to build a global network of collaborators.
“The fact that one of the co-senior authors, Dr. Tahlita Zuiverloon, who is now a faculty urologic surgeon at Erasmus University Medical Center in the Netherlands, was a postdoctoral fellow in my lab and the other, Dr. James Costello, who is a professor of pharmacology at the University of Colorado, is someone I helped recruit when I was the cancer center director there, is what makes this study particularly satisfying. We’re very excited about the future because we have a number of bladder cancer projects in the works that we hope will alter clinical practice.
Theodorescu is well-known all over the world for his research into the molecular mechanisms that cause bladder cancer and how it responds to different treatments. He is credited with the disclosure of qualities that direct cancer development and malignant growth spread and novel biomarkers that permit designated ways to deal with therapy. He has discovered effective combination therapies to target tumors that are resistant to standard immunotherapy and developed new medications for bladder and other types of cancer.
As a subsequent stage in their BRS3 research, Theodorescu and individual specialists have started a subsequent report following high-risk non-muscle obtrusive bladder malignant growth patients after some time.
According to Theodorescu, “The purpose of this new trial is to further determine whether BRS3 can help us predict patients’ responses to treatment.” We believe that this marker can also assist us in investigating alternatives to BCG treatment and, in the long run, increase the survival rates and outcomes of patients with non-muscle invasive bladder cancer.”
More information: Florus C. de Jong et al, Non–muscle-invasive bladder cancer molecular subtypes predict differential response to intravesical Bacillus Calmette-Guérin, Science Translational Medicine (2023). DOI: 10.1126/scitranslmed.abn4118