The task of combating disease cells can deplete lymphocytes used in immunotherapy therapies, or they can close as they enter growth.Utilizing a CRISPR-put together alter with respect to these cells’ genomes, scientists at UC San Francisco and Gladstone Institutes have delivered the helpful cells stronger. The disclosure might assist with beating a central point in restricting the outcome of these promising treatments in checking both strong and fluid growth.
“We’ve prevailed with regards to designing better, more grounded, longer-lived T cells that we think will further develop therapy of both blood and strong diseases,” said Alex Marson, MD, Ph.D., who, alongside malignant growth scholar Alan Ashworth, Ph.D., FRS, drove the review, published in Nature on August 24, 2022. “It’s an illustration of how we’re utilizing the force of CRISPR to speed up the plan of further developed T-cell treatments.”
Marson also serves as the director of the Gladstone-UCSF Institute of Genomic Immunology, a joint effort of the two foundations to present a blend of cutting-edge genomic innovations as a powerful influence in the development of new cell-based immunotherapies.
“These genomic breakthroughs are opening up new avenues for addressing the challenges of developing highly effective and precisely targeted immunotherapies. The ability to direct cell behavior by manipulating the genome will almost certainly lead to transformational changes in the treatment of many diseases.”
Ashworth, president of the Helen Diller Family Comprehensive Cancer Center.
“These genomic advancements are making it possible to handle the difficulties of growing profoundly viable and exactly designated immunotherapies,” said Ashworth, leader of the Helen Diller Family Comprehensive Cancer Center. “The ability to coordinate cell conduct by controlling the genome will probably prompt groundbreaking changes in the treatment of numerous illnesses.”
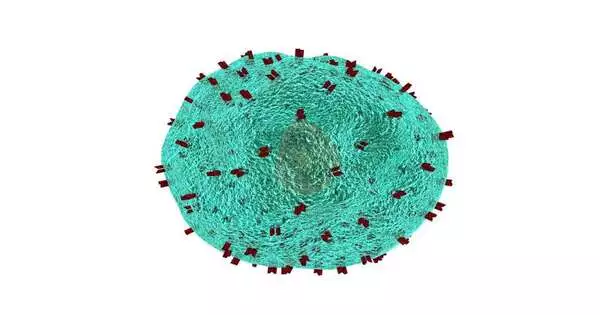
One of the significant difficulties of growing profoundly viable disease immunotherapies is the way that cancers exist in a climate that stifles T cells and other safe cells, permitting the growth to frame and develop. Helpful T cells, designed by a patient’s own T cells to perceive and kill growth cells, frequently get depleted or broken as they fight this climate, becoming unfit to bring down the disease cells.
Taking out one individual quality, we’ve made cells that are strong growth cell executioners as well as additional steady executioners over an extensive stretch of time, said doctor researcher Julia Carnevale, MD, a related creator on the review, who has as of late begun her own lab in UCSF’s Department of Medicine, seeking after new systems to design prevalent cell treatments for disease treatment.
A startling objective
Utilizing a bunch of CRISPR screens that permitted them to switch off every quality in the genome, each in turn, in a pool of human T cells, the group found a small bunch of competitors that could deliver the T cells impervious to key parts of the safe suppressive microenvironment frequently tracked down in growth.
Carnevale, who is likewise a member agent at Gladstone, and co-relating creator Eric Shifrut, Ph.D., were especially charmed by one quality named RASA2, on the grounds that it had never been associated with safe cell capability previously.
“This was strange T-cell science,” said Shifrut, a previous postdoctoral researcher in the Marson lab and currently a partner teacher at Tel Aviv University. “By zeroing in on RASA2, we were curious as to whether controlling articulation of quality in human T cells could make them more delicate immunotherapy specialists.”
Using models created by collaborators Giedre Krenciute, Ph.D., of St. Jude Children’s Research Hospital and Justin Eyquem, Ph.D., the team created T cells lacking the RASA2 quality.They then exposed these T cells to different “stress tests” by presenting them over and over to disease cells as well as to models of the cancer microenvironment.
They contrasted the exhibition of these cells with that of the first helpful T cells that actually contained a working RASA2 quality. Long after the first cells had lost their disease-battling capacities, the cells with RASA2 knocked out remained amazingly eager.
The results were consistent in tests on various types of engineered T cells in which the group had inhibited RASA2, as well as across cells from a diverse range of human donors and in models of both fluid and severe disease.
“The knockout cells could simply continue to kill,” said Carnevale. “Maybe we tracked down the brake in the framework, and when we take it off, we release the capability of these helpful cells.”
Working on existing treatments
Since Carnevale has a promising objective, she and her partners are exploring it in preclinical models to smooth out its viability and survey its security, a crucial part of the exploration, said Shifrut.
“We need to guarantee that when we eliminate RASA2’s slowing down impact, the T cells just perceive and go after disease cells and not beneficial cells,” he said.
In a joint effort with different labs at the foundation, the scientists are laying the basis for a clinical preliminary by consolidating various novel advances with RASA2 erasure, to further develop a generally existing T-cell treatment.
“Indeed, even in the best-case situations, immunotherapy medicines don’t work for all patients and there are numerous instances of backslide,” Carnevale said. “In the event that we can push the limit of this helpful methodology by sorting out the correct ways of reworking T cells, that sounds truly energizing.”
Carnevale and Shifrut credited the fair and purposeful CRISPR evaluating strategy for revealing this unsuspected quality, saying the methodology guides the way toward unconsidered science and widens the effect of studies like these.
Marson concurred. “This study instructed us that RASA2 plays a role in immunology that had recently been neglected,” he said. “Comparable orderly examinations, utilizing CRISPR to take a gander at each quality in the genome, won’t just speed up planning of malignant growth treatments, but ought to likewise support planning of cell meds that are better at treating a wide range of conditions, from immune system issues to irresistible illness.”
More information: Alexander Marson, RASA2 ablation in T cells boosts antigen sensitivity and long-term function, Nature (2022). DOI: 10.1038/s41586-022-05126-w. www.nature.com/articles/s41586-022-05126-w
Journal information: Nature