Depending on what a test is looking for, getting results from a blood test can take anywhere from an hour to a week. The same holds true for examinations of food and water contamination. The majority of the time, lengthy procedures in sample processing and analysis are what cause the delay.
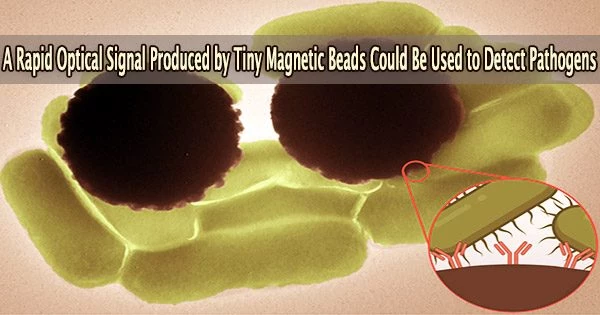
In a popular class of magnetic beads, MIT engineers have now discovered a novel optical signature that might be utilized to quickly detect impurities in various diagnostic procedures. For example, the team showed the signature could be used to detect signs of the food contaminant Salmonella.
The so-called “Dynabeads” are tiny magnetic beads that can have antibodies applied to them that bind to particular target molecules, such a particular pathogen. Dynabeads are frequently employed in investigations where they are dissolved in liquids to capture target molecules. But after that, researchers need to perform more time-consuming processes to make sure the molecules are actually there and attached to the beads.
The MIT team found a faster way to confirm the presence of Dynabead-bound pathogens, using optics, specifically, Raman spectroscopy. This optical technique identifies specific molecules based on their “Raman signature,” or the unique way in which a molecule scatters light.
Dynabeads, like fluorescent tags, have an extremely high Raman signature that can be easily recognized, according to the study’s findings. This signature, they found, can act as a “reporter.” If the signal is found, it can provide an immediate confirmation in less than an hour that the target pathogen is in fact present in a particular sample.
The team is currently working to develop a portable device for quickly detecting a range of bacterial pathogens, and has reported their results today in a special issue of the Journal of Raman Spectroscopy.
“This technique would be useful in a situation where a doctor is trying to narrow down the source of an infection in order to better inform antibiotic prescription, as well as for the detection of known pathogens in food and water,” says study co-author Marissa McDonald, a graduate student in the Harvard-MIT Program in Health Sciences and Technology. “Additionally, we hope this approach will eventually lead to expanded access to advanced diagnostics in resource-limited environments.”
Study co-authors at MIT include Postdoctoral Associate Jongwan Lee; Visiting Scholar Nikiwe Mhlanga; Research Scientist Jeon Woong Kang; Tata Professor Rohit Karnik, who is also the associate director of the Abdul Latif Jameel Water and Food Systems Lab; and Assistant Professor Loza Tadesse of the Department of Mechanical Engineering.
Salmonella is the proof of concept. You could purchase Dynabeads with E.coli antibodies, and the same thing would happen: It would bind to the bacteria, and we’d be able to detect the Dynabead signature because the signal is super strong.
Professor Loza Tadesse
Oil and water
Looking for diseased cells and pathogens in fluid samples is an exercise in patience.
“It’s kind of a needle-in-a-haystack problem,” Tadesse says.
Because there are so few of them, they must be grown in carefully monitored conditions until there are enough to study, after which their cultures must be dyed. For the complete process to produce a certain positive or negative outcome, it can take several days to a week.
Both Karnik and Tadesse’s labs have independently been developing techniques to speed up various parts of the pathogen testing process and make the process portable, using Dynabeads.
Dynabeads are minuscule beads that can be bought commercially that including an iron core that is magnetic and a polymer shell that can be coated with antibodies. The surface antibodies act as hooks to bind specific target molecules. When mixed with a fluid, such as a vial of blood or water, any molecules present will glom onto the Dynabeads.
Scientists can filter the beads out of a solution by gently guiding them to the bottom of a vial using a magnet. The beads are being further separated by Karnik’s lab into those that are and are not attached to a target molecule. “Still, the challenge is, how do we know that we have what we’re looking for?” Tadesse says.
The beads themselves are not visible by the eye. That’s where Tadesse’s work comes in. Her lab uses Raman spectroscopy as a way to “fingerprint” pathogens. She has found that different cell types scatter light in unique ways that can be used as a signature to identify them.
She and her coworkers discovered in the team’s most recent research that Dynabeads also have a distinct and potent Raman signature that can serve as an amazingly obvious beacon.
“We were initially seeking to identify the signatures of bacteria, but the signature of the Dynabeads was actually very strong,” Tadesse says. “We realized this signal could be a means of reporting to you whether you have that bacteria or not.”
Testing beacon
The researchers combined Dynabeads with water tainted with Salmonella as a practical demonstration. They evaluated how light scattered across the fluid when exposed to laser light after magnetically isolating these beads onto microscope slides. Within half a second, they quickly detected the Dynabeads’ Raman signature a confirmation that bound Dynabeads, and by inference, Salmonella, were present in the fluid.
“This is something that can be used to rapidly give a positive or negative answer: Is there a contaminant or not?” Tadesse says. “Because even a handful of pathogens can cause clinical symptoms.”
The novel method developed by the team is substantially quicker than existing approaches and makes use of components that could be modified into more compact, portable forms a goal the researchers are presently pursuing. The approach is also highly versatile.
“Salmonella is the proof of concept,” Tadesse says. “You could purchase Dynabeads with E.coli antibodies, and the same thing would happen: It would bind to the bacteria, and we’d be able to detect the Dynabead signature because the signal is super strong.”
The team is especially eager to use the test in situations like sepsis, where time is of the essence and microorganisms that cause the condition cannot be quickly discovered by standard lab testing.
“There are a lot cases, like in sepsis, where pathogenic cells cannot always be grown on a plate,” says Lee, a member of Karnik’s lab. “In that case, our technique could rapidly detect these pathogens.”
The MIT Laser Biomedical Research Center, the National Cancer Institute, and the Abdul Latif Jameel Water and Food Systems Lab at MIT supported this research, in part.