Specialists at the College of Illinois School of Veterinary Medication have shown in a mouse model that a particular kind of white blood cell, one of the body’s powerful safe guards, produces cytokines that are vital for the body to obtain resistance against contagious microbes. This finding could be instrumental in creating novel, compelling parasitic antibodies.
Regardless of antibodies being hailed as one of the best accomplishments of medication, responsible for controlling or killing various perilous irresistible sicknesses, no immunizations have been authorized to forestall or control human contagious diseases.
This need was demonstrated to be particularly lethal during the coronavirus pandemic. In countries where steroids were widely used to treat lung irritation, coronavirus patients with prior conditions, for example, uncontrolled diabetes, had a higher risk of developing deadly parasitic contaminations.
“Our findings reveal that IL-17A+ CD8+ T cell Tc17, which also expresses GM-CSF, is required for mediating fungus vaccination protection without inducing hyperinflammation. So, clearly, T cell antigen specificity—whether they target viral vs. fungal or bacterial pathogens—has a significant impact on whether they play a protective or harmful function.”
Dr. Som Nanjappa, an assistant professor of immunology at the University of Illinois.
Immune system microorganisms could deliver defensive or obsessive reactions.
“A specific kind of immune system microorganism [TH17 cells] that communicates GM-CSF [granulocyte-macrophage settlement animating factor] was connected to more noteworthy seriousness of disease in individuals contaminated with the infection that causes Coronavirus,” said Dr. Som Nanjappa, an associate professor of immunology at the College of Illinois.
“Our review shows that IL-17A+ CD8+ white blood cell (Tc17), which likewise communicates GM-CSF, is essential for intervening in contagious immunization insusceptibility without actuating hyperinflammation. So obviously, the antigen explicitness of lymphocytes—whether they target viral versus contagious or bacterial microorganisms—colossally affects whether they assume a defensive or inconvenient part. “
The article, “GM-CSF+ Tc17 cells are expected to support antibody resistance against deadly contagious pneumonia without causing unmistakable pathology,” showed up in Cell Reports on October 25. Dr. Nanjappa’s co-creators on the review are Srinivasu Mudalagiriyappa, a previous alumni understudy now a researcher with Insmed Consolidated, a worldwide biopharmaceutical organization zeroed in on serious and uncommon illnesses; Jaishree Sharma, an alumni understudy in the Branch of Pathobiology; and Miranda D. Vieson, a clinical academic administrator in the Branch of Pathobiology as well as a boarded veterinary pathologist in the school’s Veterinary Symptomatic Research facility.
Lymphocytes for parasitic immunization resistance
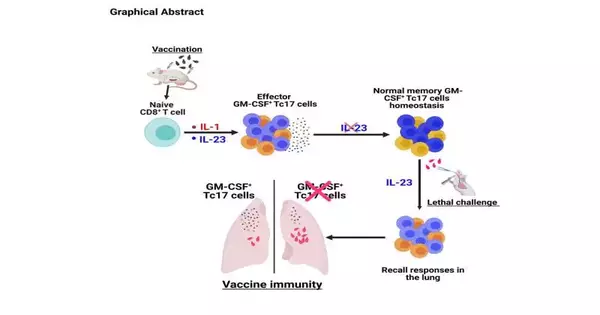
In the review, the states of mice were given a trial parasitic immunization. The mice were then presented with a harmful parasitic microbe to cause a deadly aspiratory disease. Specialists could decide whether GM-CSF+ Tc17 cells are required to intervene in antibody insusceptibility.Further, they observed that IL-1 and IL-23 cytokines are essential for evoking GM-CSF+ Tc17 cells to antibody. While IL-23 is superfluous for the long-term memory homeostasis of these cells, it is fundamental for antibody invulnerability against aspiratory contagious disease.
This study distinguishes a helpful subset of lymphocytes for contagious immunization resistance that reinforces endeavors to foster an antibody stage containing reasonable adjuvants to potentiate such a white blood cell subset.
“In accordance with this, we have distinguished a practical phenotypic marker that could be focused on to improve this subset to expand immunization viability,” said Dr. Nanjappa.
More information: Srinivasu Mudalagiriyappa et al, GM-CSF+ Tc17 cells are required to bolster vaccine immunity against lethal fungal pneumonia without causing overt pathology, Cell Reports (2022). DOI: 10.1016/j.celrep.2022.111543
Journal information: Cell Reports