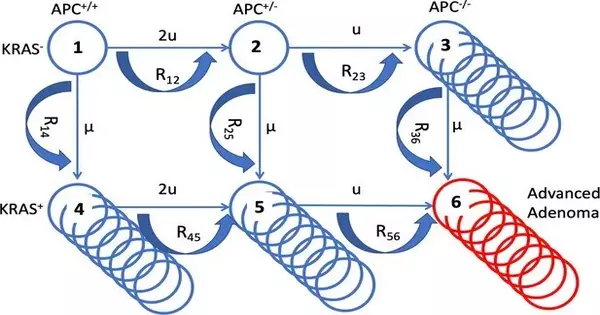
Disease begins when cells begin partitioning wildly. Researchers have realized that taking headache medicine can help safeguard against the improvement of colorectal malignant growth—a disease besetting the colon or rectum—but the specific explanation of how ibuprofen has this impact has been for the most part a secret.
In another review distributed in the journal eLife, specialists at the University of California, Irvine uncover that anti-inflammatory medicine meaningfully impacts the manner in which colorectal malignant growth cell populations develop over the long haul, making them less ready to get by and multiply.
“Cancer develops when cells transition from a healthy to a harmful state in which cells divide indefinitely. This occurs when cells acquire a number of mutations, which are then selected for. We discovered that aspirin influences and delays these evolutionary processes.”
Dominik Wodarz, professor of population health and disease
“We asked how headache medicine treats the Darwinian advancement of cells,” said co-creator Dominik Wodarz, teacher of populace wellbeing and illness avoidance at the UCI Program in Public Health. “Malignant growth emerges in light of the fact that cells develop from a sound state toward a pathogenic state where the cells partition ceaselessly.” This happens when cells secure various changes, and these transformations are chosen for We found that anti-inflammatory medicine influences these transformative cycles and dials them back. “
The group found that ibuprofen changes the birth and demise rates of colorectal cancer cells. In particular, headache medicine diminishes the pace of cancer cell division and increases the pace of cell demise.
The scientists, including the paper’s lead creator, Natalia Komarova, teacher of math, began the work thinking that ibuprofen might play a part in colorectal disease’s development wherein the powers of normal determination — or the cycles that figure out which people in a populace will get by and recreate and which will not — oversee whether malignant growth cells multiply to the point where they become unsafe or deadly.
“We believed that an eased back improvement of disease because of headache medicine should some way or another emerge from an eased back development of the cells toward danger,” said Komarova. “What astonished us was that this system could make sense of the degree of security found in the human populace very well.” At the end of the day, the anticipated extent was steady with the defensive impact found in the human populace in epidemiological examinations. “
A 2011 clinical preliminary uncovered that individuals who required 600 milligrams of headache medicine every day for quite a long time had a 63% decrease in colorectal malignant growth events in patients experiencing Lynch disorder—an acquired condition that expands one’s chance of fostering specific kinds of disease like colorectal malignant growth. Numerous different examinations substantiate those discoveries, but none as of not long ago has researched a potential transformative clarification for why this occurs.
“The original part is truly saying that headache medicine changes the transformative result of carcinogenesis,” Wodarz said. This work is a model demonstrating the way that numerical methodologies can be exceptionally valuable to grasp complex peculiarities in disease science; such bits of knowledge wouldn’t be imaginable to get by trial and error alone. It requires the cooperation of exact organic work and math. “
Presently, Komarova and the remainder of the group want to know whether anti-inflammatory medicine likewise affects diseases burdening different organs in the body. “If not,” she inquired, “in which organs is anti-inflammatory medicine defensive, and how is it that we could make sense of these distinctions in the capacity to safeguard against malignant growth?”
More information: Yifan Wang et al, Aspirin’s effect on kinetic parameters of cells contributes to its role in reducing incidence of advanced colorectal adenomas, shown by a multiscale computational study, eLife (2022). DOI: 10.7554/eLife.71953