Byproducts of the gut microbiota circulate in the bloodstream, affecting host physiological systems such as immunity, metabolism, and brain functioning. Scientists from the Institut Pasteur (a Université Paris Cité partner research organization), Inserm, and the CNRS discovered that hypothalamic neurons in an animal model directly sense differences in bacterial activity and modify hunger and body temperature accordingly. These findings show that there is direct communication between the gut microbiota and the brain, which could lead to new therapeutic methods for metabolic illnesses such as diabetes and obesity. The findings have been published in the journal Science.
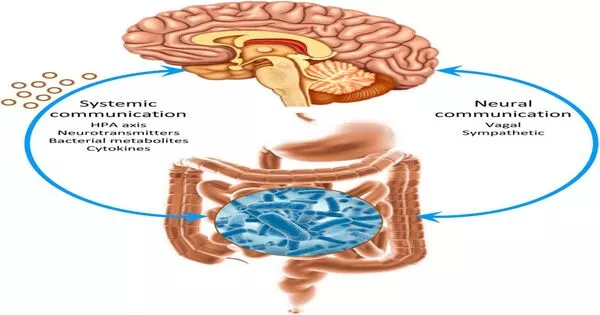
The gut is the body’s greatest bacterial reservoir. A rising body of research demonstrates the degree of connection between hosts and their gut microbiota, emphasizing the significance of the gut-brain axis. Neurobiologists from the Perception and Memory Unit (Institut Pasteur/CNRS), immunobiologists from the Microenvironment and Immunity Unit (Institut Pasteur/Inserm), and microbiologists from the Biology and Genetics of the Bacterial Cell Wall Unit (Institut Pasteur/CNRS/Inserm) collaborated at the Institut Pasteur to investigate how bacteria in the gut control the activity of specific neurons in the brain.
“Muropeptides in the gut, blood and brain are considered to be markers of bacterial proliferation,”
Ivo G. Boneca, Head of the Biology and Genetics of the Bacterial Cell Wall Unit at the Institut Pasteur (CNRS/Inserm)
The researchers concentrated on the NOD2 (nucleotide oligomerization domain) receptor, which is present primarily in immune cells. This receptor detects the presence of muropeptides, which are the bacterial cell wall’s building blocks. Furthermore, it has previously been proven that variations in the gene code for the NOD2 receptor are linked to digestive problems such as Crohn’s disease, as well as neurological and behavioral disorders. These findings, however, were insufficient to establish a direct link between neuronal activity in the brain and bacterial activity in the stomach. This was uncovered in a recent study by a group of scientists.
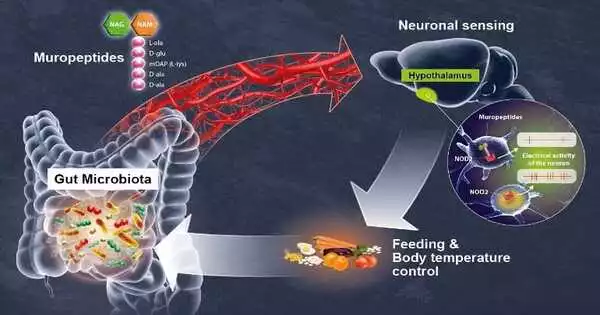
Using brain imaging techniques, the scientists discovered that the NOD2 receptor in mice is expressed by neurons in several parts of the brain, particularly the hypothalamus. They later observed that when these neurons come into contact with bacterial muropeptides from the stomach, their electrical activity is reduced. Muropeptides in the gut, blood, and brain are thought to be markers of bacterial proliferation, “Ivo G. Boneca, Head of the Biology and Genetics of the Bacterial Cell Wall Unit at the Institut Pasteur (CNRS/Inserm), explains. Muropeptides no longer inhibit these neurons if the NOD2 receptor is not present. As a result, the brain loses control of food consumption and body temperature.
The researchers proved in this work that neurons directly perceive bacterial muropeptides, despite the fact that this task was previously assumed to be exclusively assigned to immune cells. “It is extraordinary to discover that bacterial fragments act directly on a brain center as strategic as the hypothalamus, which is known to manage vital functions such as body temperature, reproduction, hunger, and thirst,” says Pierre-Marie Lledo, CNRS scientist and Head of the Perception and Memory Unit at the Institut Pasteur.
As a result, the neurons appear to detect bacterial activity (proliferation and death) as a direct indicator of the influence of food consumption on the intestinal environment. Excessive consumption of a specific food may drive disproportionate growth of some bacteria or pathogens, compromising intestinal equilibrium, explains Gérard Eberl, Head of the Microenvironment and Immunity Unit at the Institut Pasteur (Inserm).
The effect of muropeptides on hypothalamic neurons and metabolism raises questions about their possible participation in other brain functions, and it may aid in understanding the link between specific brain illnesses and NOD2 genetic variations. This discovery opens the door to new multidisciplinary initiatives at the intersection of neurology, immunology, and microbiology and, ultimately, novel therapeutic approaches to brain diseases and metabolic disorders like diabetes and obesity.