Gulf War Illness is a term used to describe a variety of chronic symptoms experienced by some Gulf War veterans, including fatigue, pain, cognitive issues, and gastrointestinal issues, among others. Scientists challenge a long-held theory about a mysterious illness afflicting Gulf War veterans, providing the first direct evidence that symptoms are caused by mitochondrial dysfunction.
Gulf War Illness (GWI) is a chronic multisymptom health condition that affects one-third of all veterans who served in the Gulf War in 1991, with the majority still suffering more than 30 years later. Fatigue, headaches, muscle aches, joint pain, diarrhea, insomnia, and cognitive impairment are all common symptoms.
Veterans’ exposure to environmental toxins is thought to have triggered the condition. However, its exact mechanism in the body is still unknown, making diagnosis and treatment difficult. The prevalent belief is that inflammation is the root cause of the symptoms, as inflammatory markers in affected veterans are slightly higher than in healthy controls. A competing theory contends that mitochondria, the energy-producing organelle found in all cells, are the true source of the symptoms.
This is a radical rethinking of the pathology of GWI. For veterans who have long struggled to get effective care, this discovery could be a real game changer.
Beatrice Golomb
In a new study, researchers at University of California San Diego School of Medicine put both ideas head-to-head, directly assessing mitochondrial impairment and inflammation in 36 individuals, 19 of whom were veterans with GWI. The findings, published July 12, 2023 in Scientific Reports, suggest that impaired mitochondrial function, and not inflammation, is the main driver of GWI symptoms and should be the primary target of future clinical interventions.
“This is a radical rethinking of the pathology of GWI,” said corresponding author Beatrice Golomb, MD, PhD, professor of medicine at the University of California, San Diego. “For veterans who have long struggled to get effective care, this discovery could be a real game changer.”
The researchers collected muscle biopsies from study participants and measured mitochondrial respiratory chain function (MRCF) levels to assess the roles of mitochondrial function and inflammation in GWI. Participants’ blood levels of high-sensitivity C-reactive protein (hsCRP), a common marker of peripheral inflammation, were used to assess inflammation.
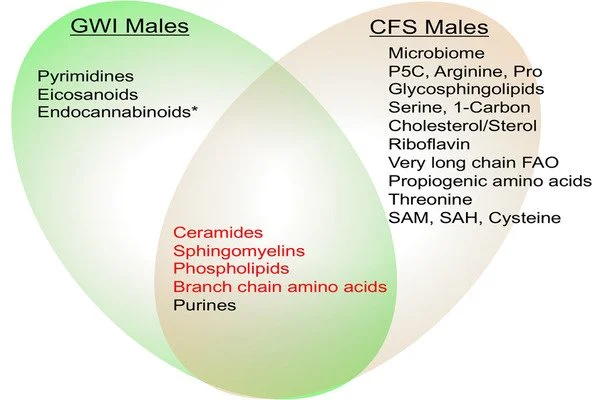
The researchers then compared this data to the participants’ GWI symptoms and found that the severity of symptoms could be predicted by their degree of mitochondrial impairment, but not by their degree of inflammation. Further statistical analyses found that 17 of the 20 most common GWI symptoms were statistically related to mitochondrial function. In contrast, only one of the 20 symptoms met this criterion for inflammation.
Another set of analyses revealed that the degree to which participants’ mitochondria were compromised in converting fat to energy was strongly related to the degree of inflammation in GWI patients, but not in controls. Reduced activity of this process, called fatty acid oxidation, is known to trigger cell death, which then leads to inflammation. Thus the researchers say this suggests that mitochondrial dysfunction may be the reason inflammation is higher in GWI patients.
“Inflammation does appear to be linked to GWI, but our work suggests that it’s actually a side effect of the primary issue, which is impaired cell energy,” said Golomb.
Many GWI symptoms, according to the researchers, are expected outcomes of mitochondrial dysfunction. Muscles, for example, rely heavily on fat for fuel, so if mitochondrial dysfunction leads to impaired fatty acid oxidation in GWI patients, this could explain their frequent muscle aches and physical fatigue. Indeed, muscle symptoms in GWI were most strongly related to the degree of mitochondrial fatty acid oxidation impairment. The brain, on the other hand, relies heavily on sugar for energy, and brain symptoms in GWI were most strongly linked to impairment in mitochondrial energy production using sugar as a fuel.
The findings may also have implications for other health conditions such as toxin exposure, aging, and even heart disease. Many of these conditions are characterized by increased inflammation, but they frequently do not respond well to anti-inflammatory medications. Golomb and colleagues contend that mitochondrial dysfunction may be an underlying cause of these conditions, opening the door to new therapeutic strategies.
“This is the first time that direct evidence for the mitochondrial hypothesis of GWI has been reported,” Golomb explained. “We hope that it will lead to improved treatment plans for the veterans who have long struggled with this mysterious illness.”