Notwithstanding progress in treatment for elevated cholesterol, coronary illness remains the main cause of death in the U.S. Researchers at the Clinical School of Wisconsin (MCW) are exploring the role of a type of cholesterol called exceptionally low-thickness lipoprotein, and their discoveries might prompt new treatment choices later on.
The examination group is driven by Ze Zheng, MBBS, Ph.D., MCW aide teacher of medication (endocrinology and sub-atomic medication); co-head of the MCW Cardiovascular Center’s Atherosclerosis, Apoplexy, and Vascular Science Program; and partner agent at Versiti Blood Exploration Establishment. As of late, the group’s discoveries were distributed in Science, where Dr. Zheng filled in as the paper’s senior creator.
François Poulletier de la Salle effectively separated cholesterol from a gallstone in 1769, when his friends accepted that blood contained just a single protein and no fat. Researchers worked frantically to characterize its sub-atomic recipe and shape and better figure out its association with the gathering of plaque in veins and the advancement of coronary illness. The primary statin was supported by the Food and Drug Administration (FDA) in 1987 to treat patients with elevated cholesterol and lessen their risk of enduring coronary episodes and strokes. In 2015, the FDA supported another sort of medication, known as proprotein convertase subtilisin-kexin type 9 inhibitors, to give cardiologists one more apparatus for patients whose cholesterol levels are still too high after treatment with statins alone.
“It is clear that there is more going on than what statins and these newer inhibitor drugs can control. More therapies are required, and in order to obtain them, we need to learn more about other sources of risk for heart disease, particularly heart attacks and strokes.”
Ze Zheng, MBBS, Ph.D., MCW assistant professor of medicine (endocrinology and molecular medicine;
However, coronary illness is as yet the main source of death in the U.S., as per the Communities for Infectious Prevention and Counteraction, and stroke keeps on being a significant issue as the fifth driving reason for death. One clinical preliminary study following patients taking proprotein convertase subtilisin-kexin type 9 inhibitors showed an advantage while likewise uncovering a chance for development as the outright gamble decrease was viewed as unassuming at 1.5%.
Obviously, there is more happening than exactly what statins and these newer inhibitor medications have some control over,” says Dr. Zheng. “More treatments are required, and to get them, we really want to find out about different wellsprings of hazard for coronary illness, particularly respiratory failures and strokes.”
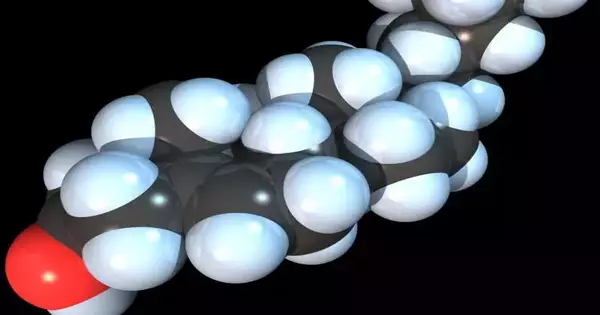
A few types of cholesterol flow in our circulation system. The sort ordinarily alluded to as “terrible cholesterol” is conveyed by a protein called apolipoprotein B (apoB), which structures very organized particles with lipids and proteins. These particles act as steady vehicles for moving lipids like cholesterol in the circulatory system. These lipid-rich particles, for the most part, incorporate extremely low-thickness lipoprotein (VLDL) and low-thickness lipoprotein (LDL). The ongoing medications for lowering cholesterol decrease LDL levels. While significant proof shows that LDL is vital to control, it isn’t the main risk factor for coronary illness. As a matter of fact, different lipoproteins in a similar group as LDL are not diminished by much with accessible medicines. Dr. Zheng and his group are researching how to decrease levels in different individuals of this group of lipoproteins, particularly VLDL.
“With my experience in lipid digestion, I ended up reliably checking lipid levels in any event, during studies in regards to blood cluster lysis and how a disability in the body’s capacity to eliminate blood clumps influences the risk of vein blockages,” Dr. Zheng adds. “I was simply normally inquisitive about it, and I saw that a protein I was examining may affect how much cholesterol flows.”
In earlier explorations, Dr. Zheng has characterized another cell wellspring of this protein, tissue-type plasminogen activator (tPA), and its job in separating blood clumps and forestalling vein blockages. To comprehend its expected effect on cholesterol levels, her group utilized a quality-altering procedure to prevent liver cells from creating tPA in mice inclined to vein plaque development. The researchers found that the mice created expanded lipoprotein cholesterol in this trial and afterward approved the discoveries in follow-up examinations utilizing human liver cells and a kind of rodent liver cell known to deliver VLDL in a manner similar to human liver cells. With these and other exploratory outcomes distributed in Science in September 2023, Dr. Zheng and her group have exhibited a new, significant finding that liver tPA impacts blood cholesterol levels while highlighting a significant association between the liver, heart, and veins.
“In the wake of characterizing this new job for tPA, we directed our concentration toward the subject of how it changes blood cholesterol levels,” notes Wen Dai, MD, research researcher at the Versiti Blood Exploration Establishment.
The liver adds to most of the “terrible” apoB-lipoproteins by making VLDL. The group zeroed in on whether and what tPA means for the course of VLDL gathering in the liver. Microsomal fatty substance move protein (MTP) is expected for the gathering of VLDL because of its job of conveying lipids to the apoB. The researchers verified that tPA ties with the apoB protein in a similar spot as MTP. The more tPA is available, the fewer doors MTP needs to open to associate with apoB and catalyze the production of new VLDL. In the event that MTP is the quarterback attempting to pass a cholesterol football to an open apoB collector, then tPA is the cornerback separating the play.
“In view of our earlier examination, we realized it was additionally basic to take a gander at tPA’s essential inhibitor,” Dr. Zheng says.
Plasminogen activator inhibitor-1 (PAI-1) is known to obstruct the movement of tPA. Researchers have likewise tracked down a connection between PAI-1 levels in the blood and the improvement of sickness because of plaque development and blockages in veins. The group tracked down that higher levels of PAI-1 diminished the capacity of tPA to bind with apoB proteins, making tPA less powerful at rivaling MTP to forestall VLDL creation. Getting back to the organic turf, PAI-1 may be an imitation collector that occupies tPA until MTP interfaces with apoB for a major increase. The group concentrated on this connection in human subjects with a normally occurring transformation in the quality conveying the code for PAI-1. The scientists tracked down that these people, as anticipated, had higher tPA levels and lower LDL and VLDL levels than people from a similar local area who didn’t have a similar transformation.
“We are researching remedial techniques in view of these discoveries in regards to tPA, MTP, and PAI-1,” Dr. Zheng notes. “I figure we might have the option to decrease the remaining cardiovascular risk that has continued even as treatment has progressed.”
More information: Wen Dai et al, Intracellular tPA–PAI-1 interaction determines VLDL assembly in hepatocytes, Science (2023). DOI: 10.1126/science.adh5207