The most vital step in picking the proper therapy for a disease patient is to recognize their particular sort of malignant growth, including deciding the essential site — the organ or part of the body where the disease starts.
In uncommon cases, the beginning of a disease is not set in stone, even with broad testing. Although these tumors of obscure essential will generally be forceful, oncologists should treat them with non-designated treatments, which regularly have cruel poison levels and result in low rates of endurance.
Another profound learning approach created by scientists at the Koch Institute for Integrative Cancer Research at MIT and Massachusetts General Hospital (MGH) may assist with ordering tumors of obscure essential by investigating the quality articulation programs connected with early cell improvement and separation.
At times, you can apply every one of the devices that pathologists bring to the table, and you are still left without a response, says Salil Garg, a Charles W. (1955) and Jennifer C. Johnson Clinical Investigator at the Koch Institute and a pathologist at MGH. “AI devices like this one could help oncologists choose more viable medicines and give their patients more direction.”
“Sometimes you may use all of the tools available to pathologists and still come up empty-handed. Such machine learning technologies might enable oncologists to select more successful therapies and provide more information to their patients.”
Salil Garg, Investigator at the Koch Institute and a pathologist at MGH.
Garg is the senior creator of another review, published Aug. 30 in Cancer Discovery. The man-made reasoning device is fit for recognizing disease types with a serious level of responsiveness and precision. Garg is the senior creator of the review, and MIT postdoc Enrico Moiso is the lead creator.
Artificial intelligence is being developed.
Parsing the distinctions in the quality of articulation among various types of cancers of obscure essential is an ideal issue for AI to settle. Disease cells look and act uniquely in contrast to typical cells, to some degree due to broad changes in how their qualities are communicated. Because of advances in single cell profiling and endeavors to list different cell articulation designs in cell map books, there is abundant — if, to natural eyes, overpowering — information that contains signs of how and from where various tumors began.
Nonetheless, building an AI model that uses distinctions among sound and typical cells, and among various types of disease, into an indicative device is a difficult exercise. In the event that a model is excessively perplexing and represents such a large number of elements of disease quality articulation, the model might seem to get familiar with the preparation information impeccably, yet waver when it experiences new information. Nonetheless, by working on the model by limiting the quantity of elements, the model might miss the sorts of data that would prompt exact orders of disease types.
To find some kind of harmony between lessening the quantity of elements while as yet removing the most important data, the group zeroed in the model on indications of changed formative pathways in disease cells. As an incipient organism creates and undifferentiated cells practice into different organs, a huge number of pathways coordinate how cells partition, develop, change shape, and move. As the growth creates disease, cells lose large numbers of the specific qualities of developed cells. Simultaneously, they start to look like early stage cells here and there, as they gain the capacity to multiply, change, and metastasize to new tissues. Large numbers of the quality articulation programs that drive embryogenesis are known to be reactivated or dysregulated in disease cells.
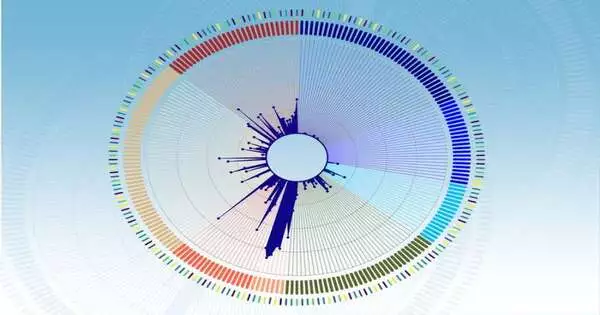
The analysts analyzed two huge cell map books, recognizing connections among growth and early-stage cells: the Cancer Genome Atlas (TCGA), which contains quality articulation information for 33 growth types, and the Mouse Organogenesis Cell Atlas (MOCA), which profiles 56 separate directions of undeveloped cells as they create and separate.
“Single-cell goal devices have decisively changed how we concentrate on the science of disease, yet the way that we make this upset effective for patients is another inquiry,” makes sense of Moiso. “With the rise of formative cell map books, particularly those that emphasize the early stages of organogenesis, such as MOCA,” we can expand our instruments beyond histological and genomic data and entryways to better approaches for profiling, recognizing growth, and developing new medicines.”
The subsequent guide of connections between formative quality articulation designs in cancer and undeveloped cells was then changed into an AI model. The scientists broke down the quality articulation of growth tests from the TCGA into individual parts that relate to a particular mark of time in a formative direction, and relegated every one of these parts to a numerical worth. The scientists then fabricated an AI model, called the Developmental Multilayer Perceptron (D-MLP), that scores growth for its formative parts and afterward predicts its starting point.
Ordering cancer
Subsequent to preparing, the D-MLP was applied to 52 new examples, especially testing tumors of obscure essentials that couldn’t be analyzed utilizing accessible apparatuses. These cases addressed the most difficult cases seen at MGH north of a four-year time span starting in 2017. Excitingly, the model classified the growth into four classifications and yielded forecasts and other data that could direct the finding and treatment of these patients.
For instance, one example came from a patient with a background marked by bosom disease who gave indications of a forceful malignant growth in the liquid spaces around the mid-region. Oncologists couldn’t find a tumor at first and couldn’t order disease cells with the tools they had at the time.In any case, the D-MLP accurately predicted ovarian malignant growth.A half year after the patient was first introduced, a mass was last observed in the ovary that ended up being the beginning of growth.
Also, the review’s precise examinations of growth and undeveloped cells uncovered promising, and at times amazing, experiences in the quality articulation profiles of explicit cancer types. For example, in the early stages of development, a simple stomach tube forms, with the lungs and other nearby organs emerging from the foregut and a large portion of the gastrointestinal system forming from the mid- and hindgut.The review showed that lung-inferred cancer cells showed solid likenesses not simply to the foregut as may be normal, but to the mid-and hindgut-determined formative directions. Discoveries like these propose that distinctions in formative projects might one day at any point be taken advantage of, similarly to how hereditary changes are usually used to plan customized or designated disease medicines.
While the review presents a strong way to deal with grouping growth, it has a few limits. In future work, analysts intend to build the prescient force of their model by consolidating different sorts of information, such as data gathered from radiology, microscopy, and different kinds of growth imaging.
“Formative quality articulation addresses just a single little cut of the multitude of elements that could be utilized to analyze and treat tumors,” says Garg. “Coordinating radiology, pathology, and quality articulation data together is the valid next stage in customized medication for disease patients.”
More information: Enrico Moiso et al, Developmental Deconvolution for Classification of Cancer Origin, Cancer Discovery (2022). DOI: 10.1158/2159-8290.CD-21-1443
Journal information: Cancer Discovery