The presence of immune cells in the body before to infection can be useful in predicting the severity of flu symptoms. Immune cells, such as T and B cells, are critical components of the immune system that assist the body in fighting illnesses such as the influenza virus.
Scientists at St. Jude Children’s Research Hospital discovered, in collaboration with the Institute of Environmental Science and Research (ESR) Limited, that immune cells present in people months before influenza (flu) infection could more accurately predict whether or not an individual would develop symptoms than current methods, which rely primarily on antibody levels. Certain immune cells were shown to be related with better protection, whereas others were found to be associated with increased vulnerability to developing symptoms after contracting the virus. The findings have implications for new approaches to public health and were published today in Nature Immunology.
“We’ve been struggling for decades, if not centuries, with why some people get sick with infections and others don’t,” said co-corresponding author Richard Webby, Ph.D., of the St. Jude Department of Host-Microbe Interactions. “This is one of the best attempts to figure out what causes influenza.” We were able to measure a variety of immunological markers from a single blood draw and connect them with immunity to illness symptoms.”
Our results show that the balance of different immune cells in people can be extremely biased. By understanding which immune cells are the best for fighting the flu, we can start designing vaccines to push for those populations that are most protective.
Paul Thomas
Functional diversity improves anti-influenza immune performance
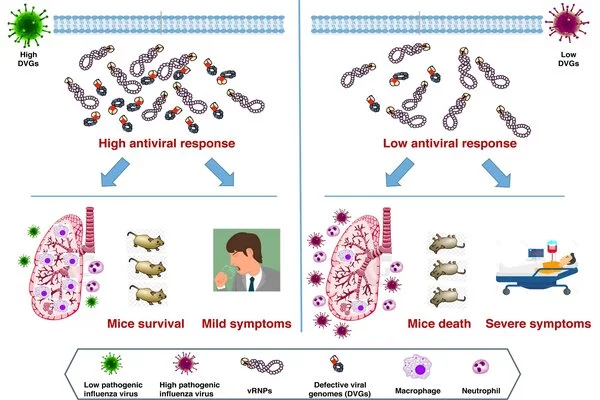
The researchers discovered that having a more functionally diversified mix of immune cells was associated with greater protection against flu symptoms. The researchers found these cells by comparing immune cells in the blood of patients with flu symptoms to those who were asymptomatic or uninfected.
Blood samples taken up to six months before the flu season revealed that the two groups had highly different sets of immune cells. Those who did not have symptoms had a more functionally diversified mix of immune cells, which were also connected with an influenza-specific long-term response, commonly known as the memory response. Patients with symptoms tended to have a more similar set of inflammatory immune cells, which are more likely to be involved in a nonspecific, functionally narrow, and short-term response.
The study comprised volunteers from a community cohort-based influenza-like illness (SHIVERS-II) study in New Zealand. SHIVERS-II comprises a unique cohort of volunteer patients who are followed over time by the study, including their health information. The volunteers in this study had their blood obtained on a regular basis so that the investigators could describe their immune cells and determine which were related with protection from flu symptoms.
“The SHIVERS platform, which represents a long-running collaboration between St. Jude and ESR, has been tremendously successful because of participants’ willingness to stay engaged in the study,” said co-corresponding author Sue Huang, Ph.D., principal investigator for SHIVERS-II and director of the World Health Organization National Influenza Centre at ESR. “It’s wonderful to see their efforts bear fruit.”
“Our results show that the balance of different immune cells in people can be extremely biased,” said senior and co-corresponding author Paul Thomas, Ph.D., St. Jude Department of Immunology. “You might build up an immune cell army that is exceptional at fighting off one kind of infection, but then that can make you feel sicker from another kind of infection. By understanding which immune cells are the best for fighting the flu, we can start designing vaccines to push for those populations that are most protective.”
“The baseline immune state before vaccination is known to vary significantly across age, sex, vaccination status, infection history, and more,” said Aisha Souquette, Ph.D., of the St. Jude Department of Immunology. “By understanding the different types of immune profiles that can provide protective responses, we can tailor and optimize our vaccine platforms for populations with distinct baseline immune states.”
Pushing for a specific type of cell or specific immune proteins, such as antibodies, is less critical for designing future personalized treatments than evaluating the collective contributions of all immune cells, which may be easier than existing methods.
“We observed that the protective, or susceptibility, cell profile’s makeup is less important than the overall, often converging, function,” said co-first author Robert Mettelman, Ph.D., St. Jude Department of Immunology. “This means that we can more broadly evaluate protection or susceptibility at the level of a cell profile, making it easier to evaluate across studies.”
Indeed, this study found that flu vaccine recipients had higher levels of protective anti-flu immune cells, increasing their chances of avoiding symptoms. Unvaccinated people who avoided symptoms appeared to have a set of immune cells that replicated the functions of protective cells in the vaccinated population. This may explain why some people are less affected by the flu than others, even when unvaccinated, but it still implies that immunization provides the best chance of avoiding symptoms. One strategy to boost vaccine uptake is to accurately quantify the inherent danger of being unvaccinated.
Improving risk predictions by adding to antibodies
With the identification of cell types associated with flu protection or susceptibility, the future promises enhanced influenza risk prediction. Anti-flu antibodies in the bloodstream have traditionally been used by clinicians and vaccine makers to predict influenza susceptibility. Antibodies are proteins that prevent viruses from infecting cells. They are created by a type of immune cell known as a B-cell. The presence of a broad mix of immune cells, with a high proportion of helper T cells, a cell engaged in the long-term immune response that “helps” B cells, was found to be more predictive of protection than antibodies alone.
“We were surprised that we could make such robust predictions just by identifying the specific cellular populations and combining it with the serological antibody data,” Thomas added. “We may already have the tools to understand infection susceptibility in our hands.” We can only accomplish it in the lab for now, but it’s startling and possibly thrilling to think that someday we might be able to readily identify at-risk folks and provide focused help.”
Aside from the predictability of cell type predictions, the time was also surprising. The samples were collected up to six months before the flu illness occurred, yet they still produced accurate forecasts, opening up new avenues for public health.
“What’s exciting is that we might be able to identify a subset of people at the start of the flu season who are more likely to get symptomatic influenza,” Webby said. “We could predict who would be at risk long before the virus was even present in the population.” I don’t think we’ve ever been in a position to even consider it before; this could open up new avenues for preventing flu-related morbidity.”
While the study’s findings may provide influenza researchers with new avenues for flu prevention, they also reaffirmed a long-standing message from virology and immunology.
“Our findings emphasize that vaccination prevents influenza symptoms, and we can now point to increased levels of those immune cells that are associated with that protection,” Thomas said. “Get your annual flu vaccine.”