Researchers have been looking for cancer treatments that are more long-lasting and effective for the past decade. Stimulator of Interfron Genes Activation (STING agonism), a promising immunotherapy that utilizes a patient’s immune system to combat tumors throughout the body, has emerged as a standout among the numerous immunotherapies.
Albeit possibly progressive, there are still basic obstacles to defeat prior to STING, and agonism can be utilized as a treatment choice for patients. For instance, the intravenous organization of STING agonist drugs is frequently not compelling because of the absence of medication strength and unfortunate take-up by insusceptible cells.
Tending to these difficulties head-on, specialists at Brigham and Ladies’ Emergency Clinic, an establishing individual from the Mass General Brigham medical care framework, have now planned upgrades to responsive nanoparticle structures, permitting STING agonist medications to be delivered while arriving at the objective cells. In a paper distributed today in Nature Nanotechnology, the specialists report that balanced Nano formulations killed dynamic cancers in mice as well as prepared their safe frameworks to perceive and dispose of future growths.
“Our goal is to use STING agonism to instruct the immune system to treat cancer cells as invaders, which necessitates the development of stable and potent nanostructures that allow STING to reach the right organs and cells,”
Ssenior author Natalie Artzi, Ph.D., a principal investigator in the Brigham’s Department of Medicine.
“We want to utilize STING agonism to teach the resistant framework to regard malignant growth cells as trespassers, which requires the plan of steady and strong nanostructures that empower STING to arrive at the right organs and the right cells,” said senior creator Natalie Artzi, Ph.D., an important specialist in the Brigham’s Division of Medication.
Lead creator Pere Dosta Pons, Ph.D., a teacher in Brigham’s Division of Medication, featured the oddity of their methodology: “We, in addition to the fact that training is the resistant framework to target and take out malignant growth cells, yet in addition to creating a safe memory for forestalling disease repeat,”
STING agonism includes the initiation of a protein called the trigger of interferon qualities (STING), which makes the invulnerable framework aware of the presence of intruders. Small messenger molecules known as cytosolic cyclic dinucleotides (CDN) attach to STING when a virus or bacterial species infects the body. This actuation prompts the creation of proinflammatory cytokines, which thusly initiate insusceptible cells like normal executioner cells, macrophages, and Lymphocytes, selecting them for the impacted region to clear the disease.
Malignant growth avoids this STING pathway by masking itself as the body’s own cells. Specialists have been endeavoring to help the resistant framework recognize and go after malignant growth cells by conveying STING agonists to safe cells in the cancer microenvironments and cancer-depleting lymph hubs.
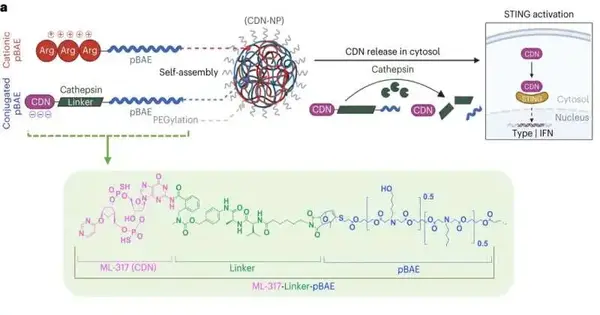
The Brigham team describes a new nanoparticle structure that makes it easier to get CDN molecules into immune cells in their latest paper. This construction straightforwardly interfaces research center-created CDNs to nanoparticles made of poly(beta amino esters), or pBAEs, making the compound more steady and intense when infused into the body, accordingly improving its remedial window. The nanostructure directs the CDN messengers to tumors and only detaches the cargo when it reaches the cells that need it.
To assess the adequacy of their methodology, the group administered CDN-nanoparticle (CDN-NP) mixtures to mice with melanoma, colon malignant growth, and bosom disease cancers. They affirmed that their CDN nanostructures were taken in by target-resistant cells in the cancer microenvironment and in auxiliary lymphoid organs, giving mice long-term susceptibility against future growths. While enduring mice were once again introduced with cancers 60 days after their underlying therapy, they had the option to dismiss the growths all alone.
The team came up with a set of design rules that must be taken into account when giving immune therapy, like how secondary lymphoid organs affect how well it works. They showed that the spleen plays a basic role in training the safe framework to produce resistant memory.
Studies like this one demonstrate the potential for enhancing gene therapy delivery systems for the treatment of diseases like cancer, in addition to addressing fundamental issues in immunology and cancer research.
“Our research addresses the fundamental interplay between the immune system and cancer through the use of a novel structure that has been designed to be both stable and potent,” Artzi stated in describing the significance of the work. In addition, we have demonstrated that targeting secondary lymphoid organs like the spleen is essential for producing a long-lasting antitumor response, which has significant repercussions for how immunotherapy is administered.”
More information: Pere Dosta et al, Investigation of the enhanced antitumour potency of STING agonist after conjugation to polymer nanoparticles, Nature Nanotechnology (2023). DOI: 10.1038/s41565-023-01447-7