Staphylococcus aureus (S. aureus) has a large number of surprises in its sack of filthy stunts, and one of the most perplexing has been the ability of non-safe types of microorganisms to emerge sound, even after exposure to high concentrations of compound fighting from antitoxins that should have the option to kill it.
That uncanny capacity of non-safe types of microscopic organisms is a stunt that permits these microorganisms to repel medications nearly as helpfully as their medication-safe partners. Ownership of medication-enduring abilities is only one of numerous problems to vex researchers who’ve been endeavoring to coax out how S. aureus tracks down ways of avoiding destructive groupings of antimicrobials.
According to the researchers, the limit of the microorganisms’ ability to remain impenetrable to strong prescriptions explains why an increasing number of patients can’t shake contaminations with non-safe strains.
“Even when the bacteria are not antibiotic resistant, Staphylococcus aureus can produce infections that are often chronic and difficult to treat.”
Dr. Markus Huemer, lead author of a new study.
“Staphylococcus aureus can cause contaminations that are frequently ongoing and challenging to treat, in any event, when the microscopic organisms are not anti-microbial safe,” reports Dr. Markus Huemer, lead creator of another review that zeroes in on the organic components undergirding the capacity of S. aureus to defeat anti-toxins.
Huemer, an examiner in the Branch of Irresistible Sicknesses and Emergency Clinic The study of disease transmission at the College Emergency Clinic in Zurich worked with a global group of microbiologists to uncover how a perplexing outpouring of synthetic exercises evidently shields the microorganisms from anti-toxin attack. The finding may ultimately assist specialists in vanquishing diseases brought about by non-safe yet complex types of microbes that regularly penetrate human tissues and the circulation system.
S. aureus is a disease-causing bacterium, and there are many strains equipped for invading human tissues and the blood. However, S. aureus additionally mystifyingly colonizes the nasal sections of around 30% of individuals in the world as a component of their microbiome. The ability of a generally irresistible bacterium to colonize without causing contamination has all the earmarks of being constrained by the creation of these people’s nasal microbiota.
The intricacy of S. aureus doesn’t end there, since more concerning are the medication-safe types of the microorganisms, deadly threats known as MRSA, or methicillin-safe S. aureus, as well as VISA, or vancomycin-middle of the road S. aureus, and VRSA, or vancomycin-safe S. aureus.
MRSA represents a danger in medical service settings, yet in networks, it’s sent to exercise centers, storage spaces, schools, and endless other places where individuals gather.
According to the United States Habitats for Infectious Disease Prevention and Awareness, S. aureus is the most well-known bacterial species that colonizes people, and anti-microbial safe assortments can impede patients for weeks to months, keeping them in long medical clinic stays and delaying therapies.Diseases can also be extremely dangerous.According to the CDC, nearly 120,000 S. aureus circulation system contaminations and 20,000 related deaths occur in the United States each year.
However, the certain logical riddle with respect to the microorganisms revolves around this basic inquiry: how could S. aureus endure deadly portions of strong anti-infection agents in a non-safe state? It’s a superpower possessed by microbes that aren’t even superbugs, and it’s taken a global team of researchers to fully comprehend why this ability has arisen in specific S. aureus strains.
Writing in the diary “Science Flagging,” Huemer and his associates have started to strip a portion of the secret, including S. aureus.In a progression of tests, the scientists have sorted out how these non-safe bacterial states arise. The investigation provides an intriguing new look into an important, but previously unknown, aspect of life for one of the world’s most common microbes.
S. aureus is prepared to withstand high concentrations of anti-microbials because it has developed a method to significantly slow its metabolic exercises, effectively suspending life “because most anti-toxins act only on metabolically dynamic cells,” Huemer explained.
S. aureus has found a way to slow its growth over time, a message sent all through bacterial provinces by a flagging particle when people attack S. aureus with anti-microbials.The flagging atom helps control the easing back of bacterial digestion and development, constraining S. aureus into an endurance mode by turning out to be not so much dynamic but rather more calm. At the point when the danger has passed, another particle signals the province to again turn out to be metabolically dynamic.
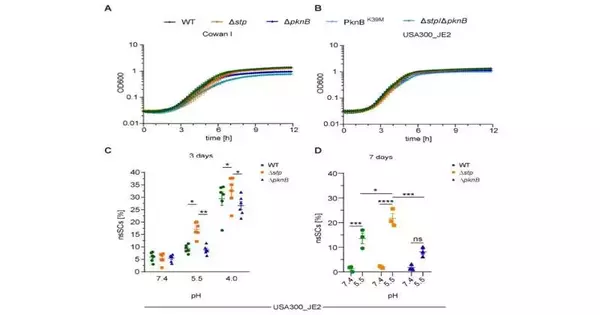
The first of these flagging atoms is known as PknB, and the second as Stp.Each plays an important role in allowing S. aureus to survive despite the compound warfare being waged against it.Perseverance — endurance — is so unpredictably part of the developmental history of the microscopic organisms that the bacterial cells obviously show how it’s done when researchers put S. aureus under brutal trial conditions.
“Subpopulations of persister cells are metabolically quiet, a state related to deferred development, diminished protein combination, and expanded resilience to anti-infection agents,” Huemer noted, showing the decreased digestion permits the microorganisms to be absolutely undeterred by the medications attacking them.
As the group knew going into the exploration, anti-microbials have their best kill rates on metabolically dynamic microscopic organisms. S. aureus, nonetheless, comes to a standstill, rising up out of the anti-infection assault.
Huemer and his colleagues discovered that these subpopulations of persister cells were made up of non-developing or super-slow-developing S. aureus while working with a variety of partners in the United States and Australia.These slow pokes enabled the bacterial state to withstand anti-toxin openness without the opposition systems discovered in settlements of extremely drug-safe microorganisms, for example, MRSA.
In their examination paper, Huemer and partners describe the persisters’ ability to rebuke anti-infection agents at the flagging organization. As a feature of their examinations, Huemer and partners exposed S. aureus to upsetting acidic circumstances, like those experienced in having tissues.
The acidic circumstances postponed the development of S. aureus, and in this manner, bacterial resistance to different antitoxins expanded. The group additionally found that when the anti-toxins flood the state, the PknB atom is enacted.
Synthetically, PknB plays out a basic errand. It indicates the increase in phosphate concentrations in the amino acids serine and threonine.The addition of phosphate groups to these amino acids reduces bacterial metabolic activity.At the point when the danger is gone, another particle, Stp, switches the movement of PknB, permitting the microbes to become dynamic once more. Huemer and his colleagues examined their perceptions using sophisticated instruments.
“We identified focuses of serine-threonine phosphorylation that may direct bacterial development and digestion using phosphopeptide advancement and mass spectrometry-based proteomics,” Huemer wrote in Science Flagging.That implies serine-threonine phosphorylation is a vital stage for S. aureus to support itself against anti-toxins, even without the exceptionally advanced organic devices drug-safe microbes use to oppose drugs.
The group concluded their report by highlighting that a human treatment procedure can be created to intercede with the flagging cycles by changing the two middle people—PPknB and Stp. They start and stop the serine-threonine phosphorylation, going about as guards that permit S. aureus to flourish in either a threatening or neighborly synthetic climate.
Controlling them provides a method for controlling these two pathways and may be able to stop ongoing S. aureus contaminations by removing obstinate persister cells.
“Our discoveries feature the significance of phosphoregulation in intervening bacterial quiet and anti-infection resilience and propose that focusing on PknB or Stp could offer a future restorative procedure to forestall persister development during S. aureus diseases,” Huemer closed.
More information: Markus Huemer et al, Serine-threonine phosphoregulation by PknB and Stp contributes to quiescence and antibiotic tolerance in Staphylococcus aureus, Science Signaling (2023). DOI: 10.1126/scisignal.abj8194