Scientists at VCU Massey Disease Center have focused on another restorative objective for a forceful type of bosom malignant growth with restricted treatment choices.
Bosom disease is the second most common malignant growth in U.S. women, and triple-negative bosom malignant growth (TNBC) is a more forceful and dangerous type of sickness that accounts for 10-15% of all bosom cancers.
TNBC develops and spreads more quickly than other types of breast cancer and is associated with more regrettable patient outcomes, accounting for nearly 33% of all bosom disease-related deaths.
Furthermore, TNBC influences people of color excessively; people of color kick the bucket from TNBC at a fundamentally higher rate than white women, in spite of being analyzed at a more youthful age. Finding a successful treatment that functions admirably in all patients would be a significant step in tending to this difference.
“The majority of TNBC cells in our investigation were universally responsive to TAK-243’s antitumor actions. Our findings show that TAK-243 can decrease tumors in numerous organs after the disease has progressed, in addition to being effective at the local site of the primary breast cancer.”
Koblinski, director of the Cancer Mouse Models Core
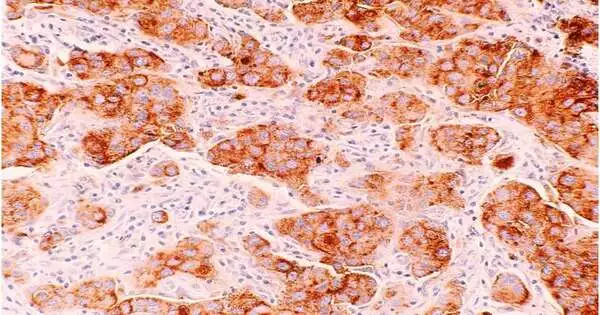
Through a complete and forefront genomic screening technique known as CRISPR/CAS9 screening, Massey researchers—driven by Anthony Faber, Ph.D., and Jennifer Koblinski, Ph.D.—had the option to recognize a particular compound called UBA1 that uncovered itself as an optimal restorative objective. Utilizing an original UBA-restraining drug called TAK-243, they impeded the phone capability of UBA1 and successfully killed malignant growth cells in persistent determined bosom cancers in mice.
Past examination has demonstrated the way that UBA1 inhibitors can have a positive effect on hematological malignant growth like intense myeloid leukemia (AML) and persistent myelogenous leukemia (CML). This review, which was recently published in PNAS Nexus, is quick to suggest that UBA1 inhibitors could be effective in TNBC.TAK-243 has been tried as of late in beginning stage preliminaries, preparing for expected testing in TNBC patients.
“We observed that most of the TNBC cells in our review were consistently vulnerable to the antitumor impacts of TAK-243,” said Koblinski, head of the Disease Mouse Models Center and individual from the Malignant Growth Science research program at Massey, as well as an academic administrator of pathology at the VCU Institute of Medication. “As well as showing this medication’s prosperity at the nearby site of the essential bosom malignant growth, our discoveries exhibit that TAK-243 can likewise shrivel cancers in different organs after the illness has spread.”
The specialists likewise resolved that the c-MYC quality — a significant and scandalously troublesome medication focus in TNBC — can be outfitted to help out TAK-243 to start a cell stress reaction and upgrade the medication’s capacity to battle TNBC. This supports the thought that TAK-243 might be successful in high-cMYC-communicating TNBC, where c-MYC might act as a biomarker for reaction to the medication.
Chemotherapy remains one of only a handful of exceptional regularly used treatment choices for TNBC, with variable patient reactions and little viability.
“The execution of designated treatments—drugs that focus on a particular hereditary deformity—has been progressive in treating various diseases, including bosom malignant growth,” said Faber, co-head of the Formative Therapeutics research program and Natalie N., also, John R. Congdon, Sr. Blessed Seat in Disease Exploration at Massey, as well as an academic partner in the Philips Organization for Oral Wellbeing Exploration at the VCU School of Dentistry.
Nonetheless, the chemical receptors, estrogen receptors, or human epidermal development factor receptor 2 (HER2) that can be successfully designated in bosom malignant growth therapy are absent in TNBC, subsequently the name “triple-negative bosom disease.”
“Genomic and clinical proof proposes that the execution of designated treatments in the treatment of TNBC will require the development of likely targets,” Faber said. “Our review might have recognized a key and novel objective for the improvement of new treatments.”
He added, “Significantly, as TNBC is a significant infection with dissimilar results between dark patients and white patients, we had the option to saddle the force of new bosom malignant growth mouse models from Dark TNBC patients that were created by Dr. Koblinski’s group.” These models have been underrepresented and are significant new devices to recognize compelling treatments for dark patients. The most thrilling piece of the review was that we found TAK-243 was powerful across these models, suggesting TAK-243 or other UBA1 inhibitors could be similarly viable in all TNBC patients.
The following stages of this investigation will include investigating the use of TAK-243 in TNBC with the pharmaceutical company that is developing it and evaluating other points in the UBA1 pathway that may also show viability.
More information: Sheeba Jacob et al, Genomic screening reveals UBA1 as a potent and druggable target in c-MYC-high TNBC models, PNAS Nexus (2022). DOI: 10.1093/pnasnexus/pgac232
Journal information: PNAS Nexus