A groundbreaking new understanding of how patients with bacterial infections develop antimicrobial resistance (AMR) is provided by a University of Oxford-led study. The discoveries, distributed today in the diary Nature Correspondences, could assist with growing more powerful mediations to forestall AMR contamination in weak patients.
The review’s discoveries challenge the conventional view that individuals are by and large tainted by a solitary hereditary clone (or ‘strain’) of pathogenic microorganisms and that protection from anti-microbial treatment develops as a result of normal choice for new hereditary transformations that happen during the disease. Instead, the findings suggest that patients are frequently co-infected by multiple pathogen clones and that resistance develops instead of through new mutations but rather through selection for resistant clones that already exist.
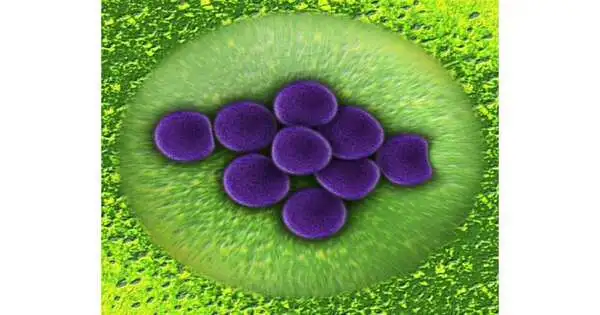
The scientists utilized a clever methodology that concentrated on changes in the hereditary variety and anti-toxin resistance of pathogenic microbes from animal types (Pseudomonas aeruginosa) gathered from patients during anti-infection treatment. The examples were isolated from 35 emergency unit patients in 12 European medical clinics. Pseudomonas aeruginosa is a shrewd microorganism that is a significant reason for medical clinic-acquired diseases, especially in immunocompromised and basically sick patients, and is remembered to cause in excess of 550,000 deaths all around the world every year.
“The main finding of this study is that selection for pre-existing resistant strains causes resistance to emerge quickly in patients colonized by various Pseudomonas aeruginosa populations. Different infections gain resistance at different rates in patients, and we hypothesize that large levels of within-host variability may be the reason why some germs, like Pseudomonas, respond quickly to antibiotic treatment.”
Lead researcher Professor Craig Maclean, from the University of Oxford’s Department of Biology,
After being admitted to the intensive care unit, each patient underwent a screening for Pseudomonas aeruginosa, and subsequent samples were collected on a regular basis. Antibiotic challenge tests and genomic analyses were used by the researchers to quantify antibiotic resistance and bacterial diversity within patients.
Most patients in the review (roughly 66%) were tainted by a solitary Pseudomonas strain. AMR developed in a portion of these patients because of the spread of new obstruction transformations that happened during contamination, supporting the regular model of opposition obtaining. The authors discovered, to their surprise, that the remaining third of patients actually had multiple strains of Pseudomonas.
Essentially, obstruction expanded by around 20% more when patients with blended strain contaminations were treated with anti-toxins, compared with patients with single strain diseases. The quick expansion in obstruction in patients with blended strain diseases was driven by the regular choice of prior safe strains that were at that point present at the beginning of anti-infection treatment. These strains typically made up a minority of the microbe populace that was available toward the beginning of anti-infection treatment; however, the anti-microbial opposition qualities that they conveyed gave them a solid particular benefit under anti-microbial treatment.
Notwithstanding the fact that AMR arose all the more rapidly in multi-strain diseases, the discoveries suggest it might likewise be lost all the more quickly in these circumstances. At the point when tests from single- and blended-strain patients were refined without even a trace of anti-toxins, the AMR strains developed all the more slowly compared to non-AMR strains. This supports the speculation that AMR qualities convey wellness compromises to such an extent that they are chosen against when no anti-infection agents are available. These compromises were more grounded in blended strain populations than in single strain populations, proposing that variety inside can likewise drive the deficiency of resistance without anti-microbial treatment.
As per the scientists, the discoveries propose that mediations pointed toward restricting the spread of microscopic organisms between patients (for example, further developed disinfection and disease control measures) might be a more viable intervention to battle AMR than interventions that plan to forestall new opposition transformations emerging during contamination, like medications that decline the bacterial change rate. This is probably going to be particularly significant in settings where the contamination rate is high, like in patients with compromised resistance.
The discoveries likewise recommend that clinical tests ought to move towards catching the variety of microbe strains present in contaminations as opposed to testing for just a few microorganism confines (in light of the suspicion that the microbe populace is really clonal). Similar to how measurements of diversity in cancer cell populations can assist in predicting the success of chemotherapy, this may make it possible to make more precise predictions regarding whether antibiotic treatments will be successful or unsuccessful in particular patients.
From the Department of Biology at the University of Oxford, lead researcher Professor Craig Maclean stated: The vital finding of this study is that obstruction develops quickly in patients colonized by assorted Pseudomonas aeruginosa populations because of the determination for prior safe strains. We speculate that high levels of within-host diversity may explain why some pathogens, such as Pseudomonas, rapidly adapt to antibiotic treatment because the rate at which resistance evolves in patients varies greatly among pathogens.
He continued: Our findings emphasize the importance of developing new diagnostic methods that will make it easier to assess the diversity of pathogen populations in patient samples. The World Health Organization has listed AMR as one of the top 10 global threats to humanity’s public health. The diagnostic methods we use to study antibiotic resistance in patient samples have changed very slowly over time. When bacteria, viruses, fungi, and parasites no longer respond to medicines like antibiotics, AMR occurs, making it harder or impossible to treat infections. The rapid spread of multi-resistant pathogenic bacteria, which cannot be treated with antimicrobial medications, is of particular concern. Worldwide, AMR was linked to nearly 5 million deaths in 2019.
Teacher Willem van Schaik, Head of the Establishment of Microbial Science and Contamination at the College of Birmingham (who was not straightforwardly engaged with the review), said: ‘ This concentrate emphatically recommends that clinical symptomatic methods might be extended to incorporate more than one strain from a patient, to precisely catch the hereditary variety and anti-toxin obstruction capability of strains that colonize fundamentally sick patients. It additionally features the significance of continuous disease anticipation endeavors that mean to decrease the chance of hospitalized patients being colonized, and thusly tainted, by deft microorganisms during their emergency clinic stay.’
Sharon Peacock, Teacher of Microbial Science and General Wellbeing at the College of Cambridge (who was not straightforwardly associated with the review), said: ‘ Multidrug-safe diseases brought about by a scope of organic entities, including Pseudomonas aeruginosa, are really difficult for patient administration in ICU settings around the world. The discoveries of this study add additional proof for the crucial significance of disease avoidance and control estimates in ICUs and clinic settings, all the more broadly because they decrease the gamble of obtaining P. aeruginosa and other pathogenic living beings.’
More information: Julio Diaz Caballero et al, Mixed strain pathogen populations accelerate the evolution of antibiotic resistance in patients, Nature Communications (2023). DOI: 10.1038/s41467-023-39416-2