An investigation of mice found that dietary sugar changes the stomach microbiome, setting off a chain of events that prompts metabolic illness, pre-diabetes, and weight gain.
The discoveries, distributed today in Cell, propose that diet matters, yet an ideal microbiome is similarly significant for the avoidance of metabolic disorder, diabetes, and weight.
Diet alters the microbiome
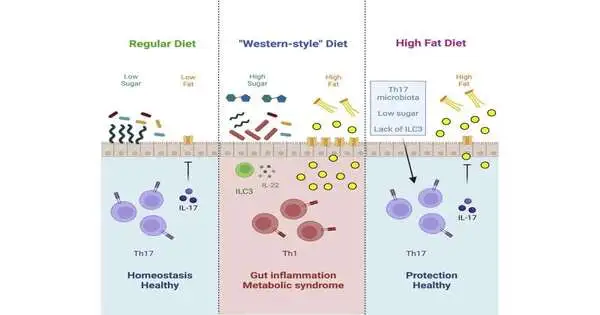
A Western-style high-fat, high-sugar diet can prompt weight gain, metabolic disorders, and diabetes, yet how the eating routine launches unfortunate changes in the body is obscure.
The stomach microbiome is key for a creature’s sustenance, so Ivalyo Ivanov, Ph.D., academic partner of microbial science and immunology at Columbia University Vagelos College of Physicians and Surgeons, and his associates examined the underlying impacts of the Western-style diet on the microbiome of mice.
Following a month on the eating routine, the creatures showed qualities of metabolic disorder, for example, weight gain, insulin resistance, and glucose bigotry. Their microbiomes had changed decisively, with how much divided filamentous microorganisms—normal in the stomach microbiota of rodents, fish, and chickens—had fallen strongly and different microscopic organisms expanding in overflow.
“These immune cells create chemicals that delay the absorption of ‘bad’ lipids from the intestines and reduce intestinal inflammation. In other words, they protect the body from absorbing pathogenic fats by keeping the stomach healthy.”
Ivalyo Ivanov, Ph.D., associate professor of microbiology & immunology at Columbia University
Microbiome changes alter Th17 cells
The decrease in filamentous microbes, the analysts found, was basic to the creatures’ wellbeing through its impact on Th17 safe cells. The drop in filamentous microbes decreased the quantity of Th17 cells in the stomach, and further tests revealed that the Th17 cells are important to forestall metabolic illness, diabetes, and weight gain.
“These safe cells produce atoms that lull the ingestion of ‘awful’ lipids from the digestion tracts and they decrease gastrointestinal irritation,” Ivanov says. “As such, they hold the stomach sound and shield the body from retaining pathogenic lipids.”
Sugar vs. fat
Which part of the great fat, high-sugar diet prompted these changes? Ivanov’s group observed that sugar was at fault.
Ivanov says that sugar kills the filamentous microbes, and the defensive Th17 cells vanish as a result. “At the point when we took care of mice with a sans sugar, high-fat eating routine, they held the digestive Th17 cells and were totally shielded from creating heftiness and pre-diabetes, despite the fact that they ate a similar number of calories.”
Yet, killing sugar didn’t help all mice. Among those coming up short on any filamentous microbes regardless, the end of sugar didn’t make a useful difference, and the creatures became fat and created diabetes.
Ivanov says that a few famous dietary mediations, for example, limiting sugar, may just work in individuals who have specific bacterial populations inside their microbiota.
In those cases, certain probiotics may be useful. In Ivanov’s mice, enhancements of filamentous microbes prompted the recuperation of Th17 cells and security against metabolic disorder, in spite of the creatures’ utilization of a high-fat eating regimen.
However, individuals don’t have similar filamentous microbes as mice, and Ivanov feels that different microorganisms in individuals might have similar defensive impacts.
Giving Th17 cells to the mice also gave security and may likewise be helpful for individuals. “Microbiota are significant, yet the genuine security comes from the Th17 cells incited by the microorganisms,” Ivanov says.
“Our review stresses that a perplexing connection between diet, microbiota, and the safe framework plays a vital part in the improvement of weight, metabolic disorders, type 2 diabetes, and different circumstances,” Ivanov says. “It implies that for optimal health, it is critical not just to change your eating regimen but also to work on your microbiome or digestive safety framework, for example, by expanding Th17 cell-actuating microorganisms.”
More information: Yoshinaga Kawano et al, Microbiota imbalance induced by dietary sugar disrupts immune-mediated protection from metabolic syndrome, Cell (2022). DOI: 10.1016/j.cell.2022.08.005
Journal information: Cell