According to a new study led by a researcher at the Boston University School of Public Health (BUSPH), if the United States had mortality rates comparable to those of other wealthy nations in 2021, it would have prevented the deaths of 1.1 million people.
The study, which was published in the journal PNAS Nexus, calls these excessive deaths “Missing Americans” because they represent people who would still be alive if US mortality rates were comparable to those of its peer nations.
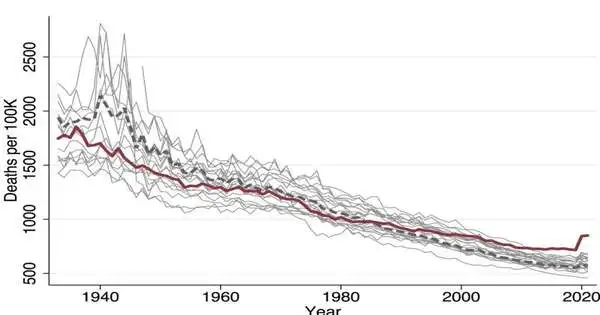
The authors find that the current death rate in the United States is significantly higher than that in 21 other wealthy nations from 1933 to 2021 and that the number of excess U.S. deaths has never been higher.
“The quantity of Missing Americans lately is extraordinary in current times,” says concentrate on lead and compare creator Dr. Jacob Bor, academic administrator of worldwide wellbeing and the study of disease transmission at BUSPH.
“Living in the United States is a risk factor for premature death that is shared by many racial and ethnic groups in the country. Whereas most health disparities studies look at differences across US racial/ethnic groups, this strategy obscures Whites’ poor health and drastically underestimates minoritized groups’ health needs.”
Dr. Jacob Bor, associate professor of global health and epidemiology at BUSPH.
In 2020 and 2021, almost 50% of all Missing Americans passed away before age 65. As per Dr. Bor, the degree of overabundance in mortality among working-age adults is especially unmistakable. “Consider individuals you realize have died prior to arriving at age 65. Genuinely, a big part of them would in any case be alive in the event that the US had the deaths of our friends. The US is encountering an emergency of early passing that is extraordinary among well-off countries.”
The COVID-19 pandemic was a big factor in the US’s sharp increase in mortality—more so than in other countries—but new research shows that the number of extra deaths in the US has been rising over the past four decades. Dr. Bor and colleagues compared age-specific mortality rates in Canada, Japan, Australia, and 18 European nations to trends in US deaths from 1933 to 2021, including the impact of COVID-19.
During and after World War II, the United States had lower mortality rates than comparable nations. During the 1960s and 1970s, the US had death rates like other rich countries; however, the quantity of Missing Americans started to increment step by step beginning during the 1980s, arriving at 622,534 yearly overabundance US passings by 2019. Passings then spiked to 1,009,467 in 2020 and 1,090,103 in 2021 during the pandemic. From 1980 to 2021, there were a total of 13.1 million Missing Americans.
The researchers emphasize that this crisis in mortality is multiracial and not restricted to marginalized groups. These measures overrepresent Black and Native Americans, whose mortality rates in early adulthood (ages 15 to 44) were five and eight times higher than those of other wealthy nations, respectively.
The group likewise says that the historical backdrop of primary prejudice in the US, including arrangements like servitude and redlining, has added to racial and ethnic differences in abundance and in admittance to schooling, lodging, and medical care that are driving reasons for higher regrettable death rates, especially at youthful ages.
Despite this, White Americans make up two-thirds of the Missing Americans. This is due to their larger population, older age distribution, and significantly higher death rates than those of other wealthy nations.
“Living in the United States is a risk factor for early death that is shared by many racial and ethnic groups in the United States. According to Dr. Bor, “such an approach renders the poor health of Whites invisible and grossly underestimates the health shortfall of minoritized groups,” “while the majority of health disparities studies assess differences between US racial and ethnic groups.”
“By using an international benchmark, we demonstrate that the US policy environment, which places a low priority on public health and social protections, particularly for low-income people,” adversely affects Americans of all races and ethnicities.
Representing future long stretches of life lost due to when an individual passes on rashly, the group gauges that in 2021, overabundance U.S. mortality will mean 26.4 million years of life lost compared with the death paces of friend countries.
According to them, the opioid epidemic, gun violence, environmental pollution, economic inequality, food insecurity, workplace safety, and the failure of US policy to adequately address major public health issues are the causes of the significant excess mortality burden. The Coronavirus pandemic exacerbated a significant number of these issues, especially among lower-paying and minority gatherings, and now that a large portion of the security net strategies made during the coronavirus have terminated, weak gatherings have lost crucial help.
“We squander many billions every year on wellbeing safety net providers’ benefits and desk work, while several millions can’t manage the cost of clinical consideration, quality food, or a fair spot to live,” says Concentrate on senior creator Dr. Steffie Woolhandler, Recognized Teacher at the School of Metropolitan General Wellbeing at Tracker School, City College of New York. “Americans die earlier than their counterparts in other countries as a result of our politicians siding with corporations when health and profits are at odds.
In contrast with the US, different nations likewise had higher immunization take-up and veil approaches during the Omicron wave, and this layered alleviation was related to fewer Coronavirus cases.
Dr. Andrew Stokes, an assistant professor of global health at BUSPH and co-author of the study, says that the findings raise a number of pressing questions that will need to be addressed in subsequent research. “Which geographic areas are disproportionately responsible for the Missing Americans, and what were their causes of death?” he asks, for instance. Replies to these inquiries might assist with explaining strategy arrangements.”
Right now, Dr. Bor says he isn’t hopeful that death rates will turn around soon, even as coronavirus-related deaths keep on fading from their 2021 peak.
“Before the pandemic began, the United States experienced an annual increase of over 600,000 missing Americans, and that number continued to rise. There have been no huge strategy changes from that point forward to adjust this course,” he says.
“The backlash unleashed during the pandemic has undermined trust in government and support for expansive policies to improve population health,” Dr. Bor stated. “While COVID-19 brought new attention to public health,” This could be the pandemic’s most damaging long-term effect because our neighbors’ countries have achieved higher life expectancy and better health outcomes by expanding public health policies.
More information: Jacob Bor et al, Missing Americans: Early death in the United States—1933–2021, PNAS Nexus (2023). DOI: 10.1093/pnasnexus/pgad173