Pacemakers, or cardiac implantable electronic devices, are used by approximately 3 million Americans. Patients’ quality of life can be significantly enhanced by these small electronic devices that are inserted into the chest or abdomen. They are typically used to treat slow or irregular heart rhythms. In any case, over the long haul, scar tissue or blood clumps can conform to the leads, or wires, that convey the electrical signals from the pacemaker to the heart.
The blockage of blood flow caused by scar tissue or blood clots may cause pain or swollen limbs. However, the prevalence and clinical consequences of lead-related venous obstruction, or LRVO, in pacemaker patients are poorly understood.
In a huge, cross-country test of government medical care recipients, doctors and scientists at the Richard A. and Susan F. Smith Community for Results Exploration in Cardiology at Beth Israel Deaconess Clinical Center (BIDMC) tracked down that the rate of suggestive LRVO among patients embedded with cardiovascular implantable electronic gadgets was multiple times higher than recently detailed, with just a minority of patients being treated with a mediation.
The specialists likewise resolved free indicators of the confusion as well as normal interventions and their results. The findings of the team were presented at the 44th annual Heart Rhythm Society Conference (HRS), which was held in New Orleans from May 19 to 21, and they were simultaneously published in the Journal of the American College of Cardiology. The goal of these two publications was to provide new information that may assist in better directing the clinical decision-making process for these patients.
“Our study expands on existing data by following patients longitudinally and identifying symptoms severe enough that invasive treatment is required; however, we believe our estimates of LRVO are likely conservative but lay the necessary foundations to understand this unrecognized but likely widespread pathology.”
Author Eric Secemsky, MD, MSc, director of Vascular Intervention at BIDMC.
Co-senior author Eric Secemsky, MD, MSc, director of Vascular Intervention at BIDMC, stated, “Although LRVO can have severe adverse effects on patients’ quality of life, the majority of existing studies only partially capture the clinical relevance of this problem.” Our review expands on existing information by following patients longitudinally and distinguishing side effects serious enough that intrusive activity is required; all things being equal, we accept our appraisals of LRVO as logically moderate, but establish the essential groundwork to grasp this unnoticed yet probable broad pathology.”
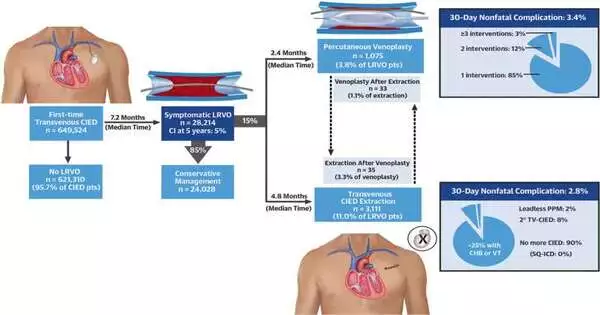
The specialists took a gander at information from almost 650,000 government medical care recipients 65 years of age and older who got a cardiovascular implantable electronic gadget somewhere in the range of 2016 and 2020 in the US. Over 28,000 patients, or five percent, were found to have LRVO within five years by the researchers.
LRVO was more common in black patients and those who also had anemia or chronic kidney disease. When the researchers looked at factors that could have predicted the onset of LRVO, they found that patients with multiple lead devices, anemia, cancer, and non-white patients were also more likely to develop LRVO.
In addition, the researchers demonstrated that conservative treatment was used by more than 85% of patients who developed LRVO; that is, they received treatment without any outside help. Three-quarters of the 15% who underwent an invasive procedure had their pacemakers removed.
Co-senior author Peter J. Zimetbaum, MD, associate chief of BIDMC’s CardioVascular Institute, stated, “Our findings showed an association between the extraction of cardiovascular implantable electronic devices and a subsequent significant reduction in LRVO-related healthcare utilization, compared to conservative management.”
“However, further prospective studies are required to define best practices for managing this underdiagnosed condition and to characterize the safety and effectiveness profiles of potential interventions that may improve patient outcomes.”
Among the patients who had their gadgets eliminated, not many got another pacemaker or defibrillator. Since leadless pacemakers are directly implanted within the heart and do not require leads, the risk of LRVO should be eliminated in just over 2% of patients who receive them. In addition, this method reduces scarring and minimizes surgical incisions. The remaining quarter underwent minimally invasive (catheter-based) procedures to either insert a stent or expand the blocked vein, but none of these procedures were associated with a decrease in healthcare use.
“There has been a proliferation of novel therapeutic options for managing LRVO that are being applied without standardization,” said first author Enrico G. Ferro, MD, a cardiology fellow at the Smith Center. “Evidence-based recommendations to guide LRVO management are needed.”
“Our data contribute to the clarification of the time course for the development and treatment of symptomatic LRVO. They also define the absolute magnitude of the problem.” Because interventions may reduce recurrent healthcare utilization, physicians may eventually be able to develop standardized treatment protocols as prompt diagnosis becomes more common.”
More information: Enrico G. Ferro et al, Incidence, Treatment, and Outcomes of Symptomatic Device Lead-Related Venous Obstruction, Journal of the American College of Cardiology (2023). DOI: 10.1016/j.jacc.2023.04.017