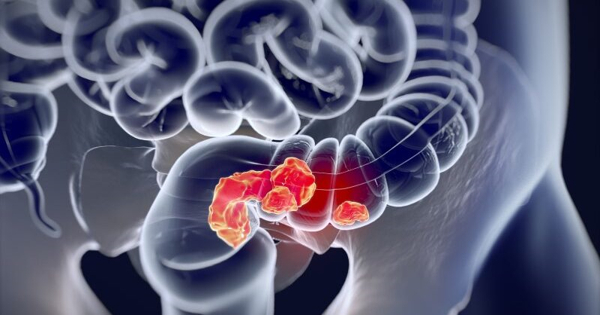
The treatment for colon cancer will be determined by how early the cancer is detected. Polyps can sometimes be removed during a colonoscopy and no additional treatment is required. Other times, surgery and/or chemotherapy may be required. A group of researchers is working on an intracavity gadget that will allow doctors to remove any remaining cancer cells during surgery, avoiding the need for extra treatments such as chemotherapy.
For those who have been diagnosed with colorectal cancer, surgery has been the only alternative that has provided a remedy. Unfortunately, when microscopic cancer cells are left behind during surgery, disease recurrence at the site of the initial tumour commonly complicates surgery. Chemotherapy is a treatment option that is often given in conjunction with surgery, although it can lead to toxic side effects.
Dr. Sung II Park, an assistant professor in the Department of Electrical and Computer Engineering and a researcher in the Center for Remote Health Technologies and Systems at Texas A&M University, and his colleagues are working to create a low-cost, minimally invasive wireless device that provides precise, safe cancer treatment options.
The biocompatible, miniaturized implantable LED device will enable light dosing and PDT that is tailored to the individual tumor response. This combination would result in a comprehensive treatment that is both safe and effective, with no hazardous side effects.
Dr. Sung II Park
The researchers will use photodynamic therapy (PDT) during surgery to kill cancer cells by utilizing a photosensitizer (a chemical triggered by light). During this approach, surgeons will be able to remove the majority of the tumor before fully irradiating the tumor bed when the photosensitizer is activated by light. This combination would result in a comprehensive treatment that is both safe and effective, with no hazardous side effects.
“The biocompatible, miniaturized implantable LED device will enable light dosing and PDT that is tailored to the individual tumor response,” Park said.
In the long run, the work will produce a platform with the potential to provide clinical-quality health monitoring capabilities for continuous use outside of traditional hospital or laboratory facilities; it will also enable treatment options to prevent the development of additional malignancies, thereby significantly improving the quality of life for people with cancer. This type of platform will help alleviate the massive fiscal burden on oncology resources, which is estimated to be $167 billion USD in 2020 alone. Global oncology spending is expected to reach $206 billion in 2022, a 23.35 percent rise.
Further details about their device are published in the issue of Nature Communications.

Colorectal cancer, excluding skin cancers, is the third most frequent cancer worldwide, according to the American Institute for Cancer Research. According to the American Cancer Society, colorectal cancer will be diagnosed in approximately 149,500 adults in the United States this year, resulting in approximately 52,980 deaths.
Although photodynamic therapy has been shown to be effective in many solid tumor cancers, its clinical application has been limited by an incomplete understanding of how cancer and normal tissue respond differently, as well as a lack of methods to monitor tumor response and adjust light dosage accordingly.
Park and his colleagues have devised a two-step technique to bridge this gap. First, a photosensitizer chemical is delivered, which is preferentially taken up by tumor cells, and then the tumor is lit with non-thermal light at a wavelength that matches the drug’s absorption spectrum. When the medication is activated, it causes a photochemical reaction that causes tumor cells to die.
“The intracavity device will provide a minimally invasive, biocompatible platform for light detection of residual cancers and delivery to tumor cells located in any part of the body, implying it could have an impact in the areas of breast, kidney, lung, pancreatic, prostate, ovarian, and rare cancers,” Park said.
Other contributors to the research include several well-known researchers from the electrical and computer engineering department, the University of Leeds and Sun Moon University.
Only six imaging modalities are available to clinicians who diagnose, stage, and treat human cancer: x-ray (plain film and computed tomography [CT]), ultrasound (US), magnetic resonance imaging (MRI), single-photon emission computed tomography (SPECT), positron emission tomography (PET), and optical imaging. Only four of these (CT, MRI, SPECT, and PET) are capable of three-dimensional (3-D) cancer detection everywhere in the human body.
Despite technological breakthroughs in many areas of diagnostic radiology, the diagnosis and imaging of human cancer remains inadequate. A major impact on cancer screening, staging, and treatment is unlikely to occur until the tumor-to-background ratio increases by three to four orders of magnitude (ie, 103- to 104-fold), which will necessitate comparable improvements in sensitivity and contrast agent targeting.