Non-thermal Atmospheric Plasma (NTAP) is a cutting-edge technology that has gained much attention in the food-processing sector over the last decade as a promising technology for food preservation and food safety, with minimal impact on food quality attributes, due to its effectiveness in microbial inactivation, including pathogens, spoilage fungi, and bacterial spores, simple design, ease of use, cost-effective operation, and short treatment time.
Non-thermal atmospheric plasma stimulates new bone formation in an animal model with critical bone defects. A recent study found that exposing an animal model to pencil-type non-thermal atmospheric-pressure plasma during surgery resulted in new bone formation in critical bone defects.
Recent technological advances that have enabled plasma to be generated at room temperature and at ambient atmosphere in what is known as non-thermal atmospheric pressure plasma (NTAPP) have allowed Japanese scientists to apply the therapeutic properties of this “fourth state of matter” to bone regeneration.
NTAPP is considered a new therapeutic method because it has been shown to accelerate cell growth when applied at low enough levels. It can generate highly reactive oxygen and nitrogen species (RONS) in the ambient atmosphere, which can be directly exposed to biological targets such as cells and tissues.
Akiyoshi Shimatani
Researchers from Osaka City University’s Graduate School of Medicine and Graduate School of Engineering discovered the utility of NTAPP in the healing of bone fractures using a pencil-type NTAPP in animal bone defect models in a study published in PLOS ONE.
“NTAPP is considered a new therapeutic method because it has been shown to accelerate cell growth when applied at low enough levels,” says first author Akiyoshi Shimatani. According to the researcher, it can generate highly reactive oxygen and nitrogen species (RONS) in the ambient atmosphere, which can be directly exposed to biological targets such as cells and tissues.
Indirect treatments have demonstrated the potential benefits of plasma in promoting the formation of stem cells that produce reactive oxygen species as well as inducing osteogenic differentiation and bone formation; however, as the team points out, there has been no report on directly using NTAPP for bone fracture therapy. “Direct exposure of NTAPP is a critical part of this study,” says Jun-Seok Oh, professor at the OCU Graduate School of Engineering and study advisor. “It required a device specifically designed to generate and deliver RONS to areas of the bone defect ‘effectively.”
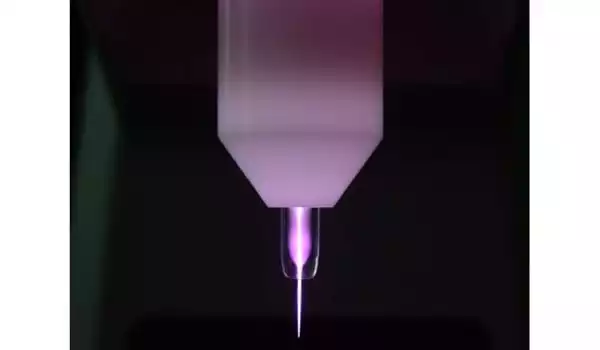
The team created a pencil-type plasma device that can effectively generate and deliver RONS to an animal model with a well-established critical bone defect, allowing them to search for the best irradiation conditions. When groups that were irradiated with NTAPP for 5, 10, and 15 minutes were compared to control groups that received no plasma, micro-CT images at eight weeks revealed that the 10-minute treatment time resulted in the most successful bone regeneration, with 1.51 times more bone volume than the control group.
“However, micro-CT images cannot tell whether a bone defect has been filled with new bone, tissue, or both,” says Hiromitsu Toyoda, an associate professor at the Graduate School of Medicine and a study co-author. As a result, the team performed a histological analysis, which revealed that “bone defects in the groups treated with plasma were filled with new bone and there was no inclusion, such as fiber tissue and gap, that was observed in the control group,” the professor continues.
The biological effect of plasma, like that of other forms of therapy, is dependent on the treatment dose delivered to the targets. Although more research is needed to determine why the 10-minute treatment period resulted in the most bone regeneration, it is known that surface wettability promotes greater cell spreading and adhesion to biomaterials and implants.
“We wondered if something similar was happening where we saw a strong generation of new bone,” says Hiroaki Nakamura, professor at the Graduate School of Medicine and study advisor, “and we found that the bone surface of the plasma-treated group was statistically and significantly more hydrophilic than the control group.”
While there is still much to be explored and understood in terms of treatment dose, the direct application of room temperature, atmospheric plasma to a living body has yielded a positive result for the first time ever. The research team hopes that the plasma device they created will be used during surgery to bring the bone regeneration effect of NTAPP to other medical fields.





