The development of new technologies for a patient’s individualized treatment is one of the major challenges in the fight against cancer. Precision medicine aims to simplify the process for cancer patients, both adults and children, to receive a customized treatment that is appropriate to their pathology based on the molecular characteristics—for example, DNA mutations—of each tumor. Can a patient’s potential to benefit from a treatment be determined before therapy even begins?
Microfluidic dynamic BH3 profiling (DBP), a microfluidic device created by a team of experts from the Faculty of Medicine and Health Sciences of the University of Barcelona and the Institute for Bioengineering of Catalonia (IBEC), predicts the effectiveness of cancer treatment quickly and automatically using a small number of cells from biopsies and without the need for specialized technical staff.
Joan Montero, professor at the UB Department of Biomedicine and IBEC, and Javier Ramón-Azcón, an ICREA research professor at IBEC, were the study’s principal investigators. It was published in the journal NPJ Precision Oncology.
“DBP has been utilized to assess the efficacy of therapy in both solid and liquid malignancies on a preclinical and clinical scale. In all cases, these research used cell lines, animal models, and primary samples with good predictive power. This assay, however, has not yet been routinely used in hospitals.”
Lecturer Joan Montero.
Albert Manzano (UB-IBEC), who received his Ph.D., is the paper’s first author. D. experts from the UB Faculty of Physics, the Vall d’Hebron Institute of Oncology (VHIO), and the Biomedical Research Networking Center in Bioengineering, Biomaterials, and Nanomedicine (CIBER-BBN) are involved in the project, which will be completed in 2022 with a thesis on precision medicine in the fight against cancer.
In the fight against cancer, precision medicine
The way we create efficient cancer treatments has been revolutionized by personalized medicine. Predictive indicators of each patient’s response to treatment are a significant advancement in oncology, given that each tumor is distinct and has its own characteristics. Professor Montero was one of the study’s co-inventors. The Dana-Farber Cancer Institute (United States) obtained a patent for dynamic BH3 profiling (DBP) in 2015. It was first created in the lab of Professor Anthony Letai.
It was one of the first functional assays to be successfully used to predict how different types of cancer would respond to treatment. With the help of this system, it is possible to quickly determine ex vivo which therapeutic approaches might be most successful in removing the tumor. Conceptually, it is very similar to the antibiograms used to find antibiotics to treat bacterial infections.
“DBP has been used to evaluate the effectiveness of therapies in both preclinical and clinical settings for a variety of solid and liquid cancers. The primary samples, animal models, and cell lines used in these studies all had a high level of predictive power. However, the use of this assay in hospitals has not yet been widely adopted, according to lecturer Joan Montero.
In primary leukemia samples, “so far, several studies have found a good correlation between DBP results and clinical response,” he continues. Several clinical trials are currently being conducted, and we hope to use this technology in hospitals in the upcoming years to enhance cancer treatments.”.
Predicting the therapeutic outcome using a small number of cancer cells.
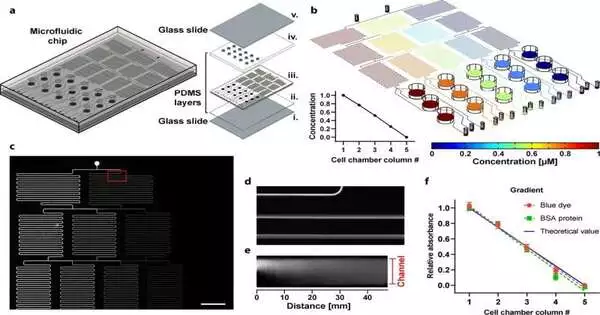
The new DBP microfluidic device, also known as the “DBP,” now addresses a number of functional assay challenges: it lowers the quantity of cancer cells required to test potential ex vivo therapies and automates the procedure to enable clinical application without the need for specialized technical staff.
“The amount of cells required to run the assay is one of the DBP’s main drawbacks.” We only get a very small number of tumor cells from a patient’s biopsy, which makes it difficult to test a wide range of treatments and makes it harder to find an effective one, according to Albert Manzano.
After receiving a biopsy, the sample is separated into individual cells using mechanical and enzymatic processes. The sample is first processed, and then it is filtered to obtain individual cells, which are then given the desired treatments and seeded in the microfluidic device.
“We can decrease the quantity of cells needed to test a treatment thanks to our DBP microfluidic platform, which is outfitted with tiny wells for seeding cells.” “This is a significant innovation that will increase the number of medications that can be tested,” continues Manzano.
An efficient system that is fully automated.
The first use of microfluidics for the functional assay of the DBP was in the paper that was published in the journal npj Precision Oncology. Unlike previous versions created, like the high-throughput DBP (Bhola et al., Science Signaling, 2020) with automated plates and dispensers to test hundreds of treatments, the new DBP device is intended to test treatments in situ in a quick, easy, and automated manner without needing expensive machinery or specialized staff.
The automation of the entire procedure, which would make it easier to apply this functional methodology on a clinical scale, is another benefit of the DBP device. The adoption of DBP as a standard trial in hospitals would be made easier by all these benefits, the experts say.
“We created this new tool with the intention of making it available to oncologists.” “We can now obtain individualized patient and treatment information thanks to this automated system,” says Javier Ramón-Azcón (IBEC).
Nanotechnology: A Revolution in Biomedicine
Numerous advancements in the design of these devices are being driven by nanotechnology, particularly the application of microfluidics to various processes in order to reduce the quantity of reagents, lower costs, automate processes, or boost the analytical capability of some methodologies, such as the DBP.
In order to facilitate the DBP analysis and gather more experimental data using primary samples to demonstrate its clinical utility in improving the treatment of various cancers, both pediatric and adult, the team is currently developing a new prototype with additional technical improvements.
“We will continue to work with our clinical collaborators to analyze patient samples and adapt this methodology to improve personalized treatment of multiple cancers for the benefit of all cancer patients,” the team’s statement from this point onward reads.
More information: Albert Manzano-Muñoz et al, Microfluidic-based dynamic BH3 profiling predicts anticancer treatment efficacy, npj Precision Oncology (2022). DOI: 10.1038/s41698-022-00333-0