Researchers from Stanford Medicine and a colleague may have discovered a potent new method for combating cancer while studying a type of bacteria that lives on every human being’s healthy skin.
They applied live Staphylococcus epidermidis bacteria to the fur of cancer-stricken mice after genetically engineering the bacteria to produce a tumor antigen—a tumor-specific protein that can stimulate the immune system. Even an aggressive form of metastatic skin cancer could be eradicated by the resulting immune response without causing inflammation.
Michael Fischbach, Ph.D., an associate professor of bioengineering, stated, “It seemed almost like magic.” We gave these mice a gentle treatment by simply applying a swab of bacteria to the fur of their heads. These mice had very aggressive tumors growing on their flanks.
“It nearly appeared magical. These mice had extremely aggressive tumors growing on their flanks, so we gave them a moderate treatment by merely rubbing a swab of bacteria on their head fur.
Michael Fischbach, Ph.D., an associate professor of bioengineering.
On April 13, their study was published online in Science. Yiyin Erin Chen, MD, Ph.D., a former postdoctoral fellow at Stanford Medicine who is now an assistant professor of biology at the Massachusetts Institute of Technology, is the lead author. Fischbach is the senior author.
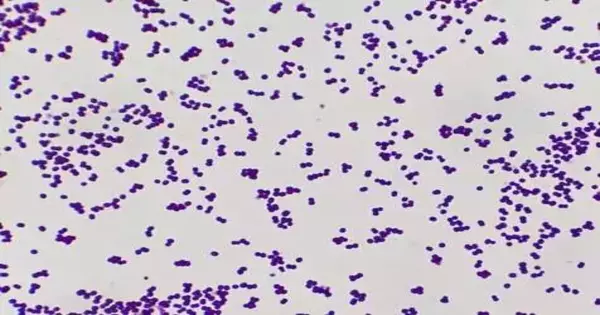
Skin colonizers Healthy skin is home to millions of bacteria, fungi, and viruses. The skin microbiota’s interaction with the immune system of the host is poorly understood, despite the fact that these friendly colonists are crucial to maintaining the skin barrier and preventing infection. Staph epidermidis, for example, is the only colonizing bacteria that causes the production of powerful immune cells known as CD8 T cells, which are the “killer” cells that fight cancer and severe infections.
By inserting a tumor antigen into Staph epidermidis, the researchers demonstrated that they could trick the immune system of a mouse into producing CD8 T cells that targeted the chosen antigen. When these cells came into contact with a tumor that was similar, they rapidly multiplied throughout the mice and either significantly slowed down or completely destroyed the tumor.
“Watching those cancers vanish—pparticularly at a site far from where we applied the microorganisms—wwas stunning,” Fischbach said. “It took us some time to accept that it was working out.”
Fischbach and his team didn’t initially set out to fight cancer; they were interested in the mystery of the T cells that do nothing. They wanted an answer to a much more fundamental inquiry: how could a host creature squander energy making white blood cells intended to go after supportive colonizing microorganisms? Particularly because these T cells are “antigen-specific,” which means that each T cell has a homing receptor that corresponds to a single bacterial fragment that activated it.
Significantly more odd, the CD8 lymphocytes incited by normally occurring Staph epidermidis don’t cause irritation; in fact, they don’t appear to do anything. Most researchers thought pilgrim-incited lymphocytes should be, in a general sense, not quite the same as ordinary white blood cells, Fischbach expressed, on the grounds that, as opposed to venturing out all through the body to chase after their objective, they appeared to remain okay underneath the skin surface, some way or another modified to maintain order among microbes and host.
The researchers engineered a strain of S. epidermidis to produce a different antigen, one that would generate T cells specific for a commonly studied tumor model in mice, in order to test whether these colony-induced CD8 T cells could behave like regular killer T cells.
They genetically grafted onto the surface of S. epidermidis a small piece of DNA encoding a portion of a protein called ovalbumin. Ovalbumin was chosen because it has been engineered into numerous well-studied mouse tumor lines, including an aggressive form of melanoma, and can thus serve as a tumor antigen in a variety of cancers.
The scientists then applied the genetically modified bacteria to healthy mice to demonstrate their effectiveness against tumor-specific T cells. They simply rubbed the bacteria on the animals’ heads because S. epidermidis is an effective skin colonizer. They did not need to clean or shave the animals’ fur. The colonization did not, as expected, result in any infection or inflammation.
As controls, different mice were treated with either no microbes, wild-type staph epidermidis (not communicating the ovalbumin peptide), or intensity, which killed ovalbumin-communicating staph epidermidis, which couldn’t colonize the skin since it was dead.
The researchers then injected the mice with ovalbumin-expressing melanoma tumor cells six days later. The mice treated with live, genetically engineered S. epidermidis grew tumors much more slowly and, in many instances, did not grow any at all, in contrast to the control mice, whose skin tumors developed rapidly in all three types.
When the researchers looked for an explanation, they discovered ovalbumin-specific CD8 T cells in the skin’s draining lymph nodes, spleen, and slowly growing tumors. According to Fischbach, these T cells must have the same immune potential as regular killer T cells.
Chen stated, “I honestly hadn’t expected it to work.” Radiation, chemotherapy, or surgery are used in every other type of tumor vaccine research, but we barely touched these mice. We were assisted by the T cells.”
15 of the 16 tumors vanished. The researchers tried injecting cancer cells up to two weeks before they colonized with the genetically engineered S. epidermidis to see if their method could treat melanoma that was already established.
Treatment with the bacteria significantly increased the mice’s chances of survival, reducing or eliminating tumors even when melanoma had spread to the lungs. When the researchers used naturally occurring melanoma antigens rather than ovalbumin, the method also worked.
The benefits were even greater when the researchers combined the new treatment with “checkpoint blockade,” a second type of immunotherapy designed to boost T cell activity: 15 out of 16 laid-out cancers vanished. Tumors remained inactive for 30 days after additional cancer cells were injected into the mice.
Fischbach stated, “This appears to be evidence of a memory immune response similar to what occurs after a vaccine.”
The specialists presently accept that the host life form creates these white blood cells to basically immunize itself against the homesteaders, safeguarding against inescapable cuts and scratches that could permit microorganisms to penetrate the skin.
Fischbach stated, “We’ve basically tricked the host into thinking that the tumor is bacterially infected.” As a result, the host is aggressively pursuing the tumor.
Additionally, the researchers tested their method in a mouse model of prostate cancer by substituting a prostate tumor antigen for the melanoma antigen. Again, the treatment significantly slowed the growth of the tumor, indicating that genetically engineered skin-colonizing bacteria can effectively fight more than just skin cancer.
Bringing treatment to people with cancer The researchers are quick to point out that cancer treatments that work in mice sometimes don’t work in people with cancer. However, Fischbach asserts that there are grounds for optimism. First, co-author Yasmine Belkaid, Ph.D., chief of the National Institutes of Health’s metaorganism immune section, demonstrated that S. epidermidis elicits the same kind of CD8 T cell response in primates as it does in mice in a previous study. Besides, while Staphylococcus epidermidis normally vanishes from mouse skin inside half a month, most people are forever colonized with some type of microscopic organism.
“Human skin is the normal home for S. epidermidis,” Fischbach said. “In people, the bug will colonize all the more effectively, possibly prompting a continually restoring supply of cancer-explicit lymphocytes.”
Other types of cancer immunotherapy involve injecting T cells back into a patient with severe side effects, engineering the T cells in the lab to produce a tumor-specific antigen, and then collecting T cells from the patient.
“We’ve found that the host is immunizing itself every day of the week against organic entities that inhabit boundary surfaces,” Fischbach said. “We will have a very effective, low-cost therapy that can simply be applied to the skin if we are able to direct even a fraction of this immune response toward specific cancers or potentially infectious diseases.”
More information: Y. Erin Chen et al, Engineered skin bacteria induce antitumor T cell responses against melanoma, Science (2023). DOI: 10.1126/science.abp9563