Pancreatic sores stand out lately on the grounds that they address one of the main forerunners of pancreatic disease recognizable through radiologic imaging. Although the majority of these sores, otherwise called pancreatic intraductal papillary mucinous neoplasms (IPMNs), will stay harmless, a subset of these neoplasms will advance to obtrusive disease. While the safe framework has been remembered to play a part in the movement of IPMNs into pancreatic disease, the particulars of its job have been hazy.
A UC San Francisco-driven group of global scientists has framed the complete safe scene and microbiome of pancreatic sores as they progress from harmless pimples to pancreatic disease. Their discoveries, published August 31 in Lancet Gastroenterology and Hepatology, could uncover the system of neoplastic movement and give focus to immunotherapy to hinder movement or treat obtrusive illness.
“This will have broad ramifications on our thought process about using immunotherapies to treat specific kinds of pancreatic disease and, furthermore, possibly hinder the arrangement and movement of malignant growth from pancreatic sores,” said senior author Ajay V. Creator, MD, FACS, FSSO, a pancreatic specialist, head of UCSF’s division of careful oncology, and Maurice Galante Distinguished Professor of careful oncology.
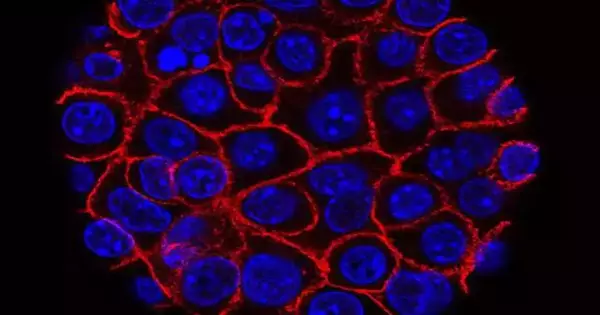
The safe cancer microenvironment of the IPMNs develops during harmful movement. A growth microenvironment is the cell climate that encompasses a cancer and incorporates safe cells and a stroma that upholds different cells and tissues. A cell’s growth and its microenvironment are continually connected with the microenvironment, impacting both sound and strange cell improvement (dysplasia).
“This could potentially prevent the development and spread of pancreatic cancer from pancreatic cysts, and it will have profound effects on how we approach using immunotherapies to treat specific forms of pancreatic cancer.”
Ajay V. Maker, MD, FACS, FSSO,
As neoplasms progress from second-rate dysplasia to high-grade dysplasia and afterward to obtrusive carcinoma, a cytotoxic safe reaction wealthy in CD8+ T cells changes to an immunosuppressive climate with a quantifiable fiery reaction.
The scientists propose that treatments that help cytotoxic T cells could be great for IPMNs with okay illness, while medicines that target administrative T cells, myeloid-determined silencer cells, and inhibitory macrophages could play a part in lessening harmful movement and treating high-risk sickness. Notwithstanding the treatment of IPMNs with a related intrusive carcinoma, tending to the safe growth microenvironment could forestall the movement of IPMNs at high risk of harmful change.
The scientists note that with moderate measures of dysplasia, the cancer microenvironment shows an expansion in the grouping of favorable to fiery and sore liquid cytokines, which is demonstrative of a T-cell immunological reaction. The group’s examination proposes that assessment and portrayal of the safe reaction to IPMNs could be considered an early finding and possibly upgraded medicines to end movement or treat obtrusive illness.
The analysts likewise propose that further examinations tending to the growth safe microenvironment of pre-obtrusive sores are required, including appraisal of primary pipe illness contrast and branch-channel sickness.
More information: Tommaso Pollini et al, The tumour immune microenvironment and microbiome of pancreatic intraductal papillary mucinous neoplasms, The Lancet Gastroenterology & Hepatology (2022). DOI: 10.1016/S2468-1253(22)00235-7