Researchers at the Public Organizations for Health and Massachusetts General Hospital Emergency Clinic in Boston have revealed a possible new methodology against liver malignant growth that could prompt the improvement of another class of anticancer medications. In a progression of examinations in cells and mice, scientists found that a protein created in liver malignant growth cells could be transformed over time by a gathering of mixtures into anticancer medications, killing cells and diminishing illness in creatures.
The specialists propose that this chemical could turn into a likely objective for the improvement of new medications against liver malignant growths and maybe other tumors and illnesses too.
“We tracked down a particle that kills cells in an uncommon liver disease in a special way,” said translational researcher Matthew Lobby, Ph.D., one of the heads of the work at NIH’s Public Community for Progressing Translational Sciences (NCATS). “It rose up from a screening to find particles that specifically kill human liver disease cells. It took a ton of work to sort out that the particle is changed over by a catalyst in these liver disease cells, making a harmful anticancer medication.”
“We believe these compounds have the potential to be an unexplored class of anticancer medicines that rely on SULT1A1 for tumor action,”
Nabeel Bardeesy, Ph.D.
Lobby, Nabeel Bardeesy, Ph.D., a liver malignant growth expert at Massachusetts General Clinic and their partners detailed their outcomes Walk 13 in Nature Disease.
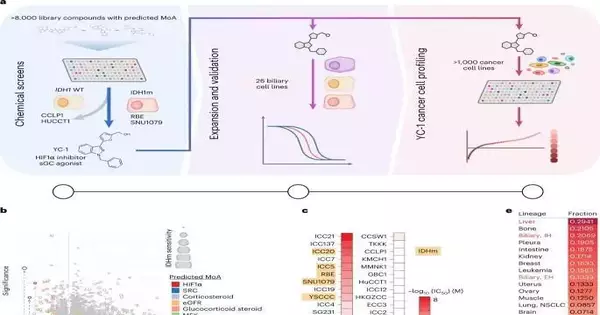
The finding originates from a coordinated effort between the Massachusetts General Medical Clinic and NCATS scientists. Bardeesy was initially contemplating cholangiocarcinoma, a type of malignant liver growth that influences the bile pipe. The malignant growth is described by transformations in the IDH1 compound. Bardeesy’s group needed to find mixtures and medications that might be powerful against the IDH1 transformation. Through their cooperation with NCATS, Lobby and other NCATS researchers quickly tried a huge number of endorsed drugs and exploratory malignant growth specialists for their viability in killing cholangiocarcinoma cells, with IDH1 as an objective.
They found a few particles, including one called YC-1, that could kill the disease cells. However, when they hoped to perceive how YC-1 was functioning, they found the compound wasn’t influencing the IDH1 transformation.
The Massachusetts scientists showed that the liver’s malignant growth cells made a catalyst, SULT1A1. The catalyst activated the YC-1 compound, making it harmful to growth cells in disease cell societies and mouse models of liver tumors. In the creature models treated with YC-1, the liver cancers either had diminished development or shrank. Alternately, the analysts found no progression in growths treated with YC-1 in creatures with disease cells, coming up short on the chemical.
The scientists analyzed different data sets of medication screening to create compound and medication libraries to coordinate medication movement with SULT1A1 action. They likewise took a gander at a huge Public Disease Foundation information base of anticancer mixtures for extra prospects to test for their action with the chemical.
They recognized a few classes of mixtures that depended on SULT1A1 for their cancer-killing action. Utilizing computational strategies, they anticipated different mixtures that were also possible and were dependent upon SULT1A1.
“When we found SULT1A1 enacting YC-1, it drove us to inquire, “What different mixtures are dynamic and can kill cells by a similar component?” Corridor said. “Might we at any point recognize different mixtures that were being created and exhibit that they were likewise dynamic due to SULT1A1 actuation? The response was yes. We tracked down different mixtures with a similar instrument of activity as YC-1.”
The researchers recommend that these discoveries have more extensive ramifications for developing new anticancer medications. “We think these atoms can possibly be an undiscovered class of anticancer medications that rely upon SULT1A1 for their movement against growths,” Bardeesy said.
The analysts see YC-1 and comparable atoms as models for creating intensifiers that could be viable against significant proteins in cells. Altering various pieces of these atoms could make them more unambiguous for such proteins. The specialists highlight the formation of a “tool compartment of SULT1A1-initiated particles” that could influence various targets.
Such a tool compartment contains many known particles. In principle, the toolbox covers many sorts of compounds, called sulfotransferases, that are dynamic in various tissues in the body. For instance, notwithstanding SULT1A1, the human sulfotransferase SULT4A1 is dynamic in the cerebrum. It can enact a subset of the particles in the toolbox. This may be helpful in creating drugs specifically for mental diseases.
“We knew SULT1A1-subordinate medications had proactively been distinguished,” Bardeesy said. “Our outcomes propose there could be other SULT1A1-subordinate mixtures with scopes for various targets. Recognizing such mixtures and focusing on cells could have possible ramifications for creating different sorts of little atoms and medications, not simply those restricted to these diseases. This could turn into another methodology for certain infections.”
More information: Lei Shi et al, SULT1A1-dependent sulfonation of alkylators is a lineage-dependent vulnerability of liver cancers, Nature Cancer (2023). DOI: 10.1038/s43018-023-00523-0