New precision medicine approaches to treating allergies in patients with high levels of Th9 are suggested by a new Nature Immunology study led by researchers from the University of Pittsburgh and the National Institutes of Health. It sheds light on how a rare type of helper T cell known as Th9 can drive allergic disease.
According to senior author Daniella Schwartz, M.D., assistant professor of rheumatology at Pitt’s School of Medicine, “Th9 cells are kind of like the black sheep of helper T cells.” They need a powerful coincidence of events to spring up, and they aren’t enduring, which makes them hard to study. Another strange thing about Th9 cells is that they continue to function even when they do not see their antigen.
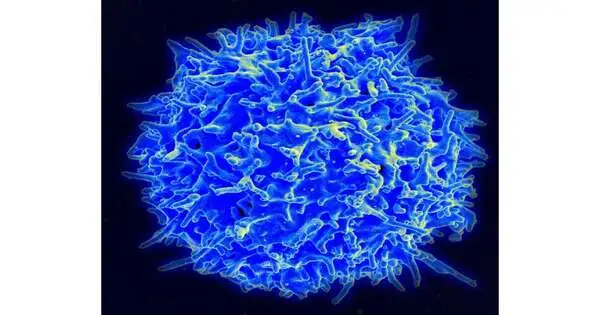
Lymphocytes switch on when they experience infections, microorganisms, or different microbes, making them increase the creation of provocative proteins called cytokines, which control a set-up of insusceptible reactions through the JAK-Detail flagging pathway. The fundamental “on” switch for lymphocytes is the point at which the immune system microorganism receptor perceives an antigen, a particular recognizing element of a danger. Bystander activation, which does not involve the T cell receptor, is an additional type of switch that exists in addition to this particular type of activation.
“They require a perfect storm of events to occur, and they aren’t long-lived, making them difficult to study. Another peculiar feature of Th9 cells is that they continue to operate in the absence of antigen.”
Senior author Daniella Schwartz, M.D., assistant professor of rheumatology at Pitt’s School of Medicine.
“Observer initiation generally requires different sorts of hazardous signs that show a danger,” said Schwartz. “Th9 cells are truly unusual because they can be activated without these harmful signals.
To study how Th9 cells are enacted in unfavorably susceptible reactions, Schwartz and her group estimated IL9, a cytokine delivered by Th9 cells, in immune system microorganisms from patients with atopic dermatitis, a hypersensitive condition portrayed by a dry, bothersome rash, and sound workers. They discovered that healthy volunteers’ Th9 cells did not respond to bystander activation like the allergy patients’ did.
According to Schwartz’s explanation, “This told us that there is some sort of checkpoint that prevents non-specific activation of Th9 cells in healthy people.” In sensitivity patients, we speculated that the designated spot separates, so you’re getting the creation of the cytokine even without restimulating the cells with antigen.”
When antigen binds to the T cell receptor in the majority of helper T cells, this highly specific recognition process causes the DNA in the nucleus of the T cell to unravel like thread on a spool, revealing regions of DNA that encode the production of cytokines, which initiate a series of immune responses. At the point when the danger is wiped out, there’s no more antigen to invigorate the immune system’s microorganism receptors, and the cells switch off. But the DNA structure is still open, so the cell is ready for a possible encounter in the future.
Schwartz and her colleagues discovered that Th9 cells regulate in a different manner. STAT5 and STAT6, transcription factors that bind to the open region of DNA around IL9 to activate the gene, activate these cells. Over time, unusually, the DNA closes, stopping IL9 production.
In healthy individuals, this mechanism for opening and closing functions as a checkpoint to manage the constantly active immune responses. Be that as it may, when this designated spot separates in sensitivity, the DNA stays open, keeping the IL9 quality turned on and driving unfavorably susceptible irritation.
In a mouse model of unfavorably susceptible asthma driven by Th9, impeding JAK-Detail motioning with a medication called tofacitinib, which is supported for treating rheumatoid joint pain, atopic dermatitis, and other fiery problems, further developed sickness side effects.
Breaking down information from hypersensitive asthma patients, the analysts found that those with more elevated levels of Th9 cells had more prominent initiation of STAT5 and STAT6-related qualities. This finding suggests new strategies for allergy precision medicine and lends credence to the hypothesis that Th9 could serve as a biomarker to identify patients who are most likely to respond to JAK inhibitors.
More information: Aran Son et al, Dynamic chromatin accessibility licenses STAT5- and STAT6-dependent innate-like function of TH9 cells to promote allergic inflammation, Nature Immunology (2023). DOI: 10.1038/s41590-023-01501-5