Researchers at the College of Virginia Wellbeing neuroscientists have found a possible method for upsetting the constant irritation liable for various sclerosis.
UVA’s new review identifies an essential supporter of the hyperactive immune system response and neuroinflammation that are symptoms of MS.Inhibiting this lynchpin in an MS test model reduced irritation, giving researchers a practical goal in developing new medicines for multiple sclerosis and other immune system illnesses.
The examination was led by Andrea Merchak, a doctoral up-and-comer in neuroscience, and her partners in the lab of Alban Gaultier of the College of Virginia Institute of Medicine’s Division of Neuroscience and its Middle for Mind Immunology and Glia, or Huge.
“Probiotics are challenging to utilize clinically due to the intricacy of the gut flora. Because this receptor is easily targeted with drugs, we may have discovered a more dependable way to foster a healthy gut flora.”
Andrea Merchak, a doctoral candidate in neuroscience,
“We are moving toward the quest for various sclerosis therapeutics under another heading,” Merchak said. “By regulating the microbiome [the assortment of microorganisms that normally live inside us], we are making advances in understanding how the resistant reaction can wind up wild in autoimmunity.” “We can utilize this data to track down early intercessions.”
Various forms of sclerosis influence almost 1,000,000 Americans. Side effects can incorporate muscle fits, solidness, shortcoming, trouble moving, wretchedness, and torment; from there, the sky is the limit. There is no fix. All things considered, medicines center around assisting patients with overseeing side effects, controlling flareups, and slowing the illness’ movement.
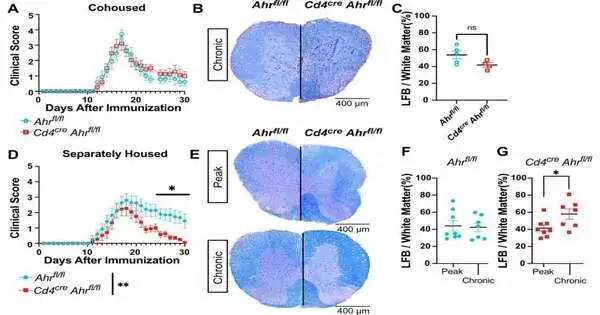
Researchers have attempted to figure out the reasons for MS; however, late exploration proposes a significant job for the stomach microbiome. That’s what UVA’s new discoveries reinforce, verifying that a resistant framework regulator viewed as “hindrance tissues,” for example, the digestive system, assumes a fundamental part in the sickness. This controller can reconstruct the stomach microbiome to advance unsafe, persistent aggravation, the analysts found.
Gaultier and his colleagues hindered the movement of the controller, called the “aryl hydrocarbon receptor,” in resistant cells called lymphocytes, which prompted a sensational impact on the creation of bile acids and different metabolites in the microbiomes of lab mice. With this receptor down and out, aggravation diminished, and the mice recuperated.
The discoveries recommend that specialists may one day have the option to adopt a comparative strategy to intrude on the destructive irritation in individuals with MS. That will take significantly more examination, notwithstanding. Researchers will require a superior comprehension of the interactions between the resistant framework and the microbiome, the UVA specialists say.
In any case, UVA’s new research provides a significant starting point for future efforts aimed at focusing on the microbiome to reduce irritation linked to multiple sclerosis and other immune system illnesses.
“Because of the intricacy of the stomach lining, probiotics are hard to clinically utilize.” “This receptor can undoubtedly be designated with prescriptions, so we might have tracked down a more dependable course to advance a sound stomach microbiome,” Merchak said. “Eventually, using the microbiome to tweak the resistant response could save patients from having to deal with the harsh side effects of immunosuppressant drugs.”
Gaultier and his associates have distributed their discoveries in the logical journal PLOS Science.
More information: Andrea R. Merchak et al, The activity of the aryl hydrocarbon receptor in T cells tunes the gut microenvironment to sustain autoimmunity and neuroinflammation, PLOS Biology (2023). DOI: 10.1371/journal.pbio.3002000